Tear in the uterine wall, in most cases during labour.
In a CEmONC or BEmONC facility, uterine rupture can be reduced by monitoring the progress of labour with partograph, and vigilant, rational use of oxytocin and prostaglandins.
3.3.1 Circumstances in which uterine rupture occurs
- Obstructed labour.
- Grand multiparas (5 deliveries or more).
- When excessive amounts of uterotonic (oxytocin or misoprostol) are used.
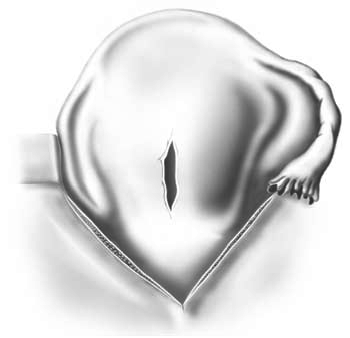
- Prior history of uterine surgery: caesarean section, especially classical (Figure 3.2); uterine perforation; myomectomy.
Figure 3.2 - Uterine rupture on a classical caesarean section scar
3.3.2 Diagnosis
Diagnosis is clinical. A rupture may be diagnosed during labour or after delivery. Though the initial symptoms may be subtle – particularly in cases of scarred uterus – the signs are usually obvious.
During labour
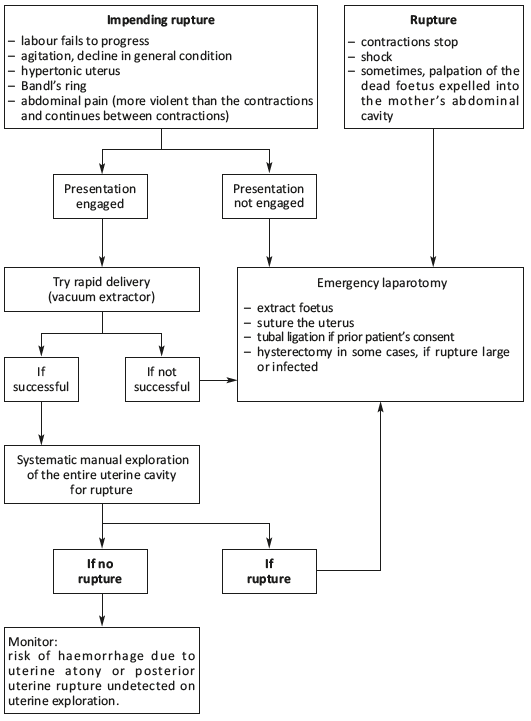
- Impending rupture:
- maternal agitation;
- increasingly severe abdominal pain that persists between contractions; abdominal guarding;
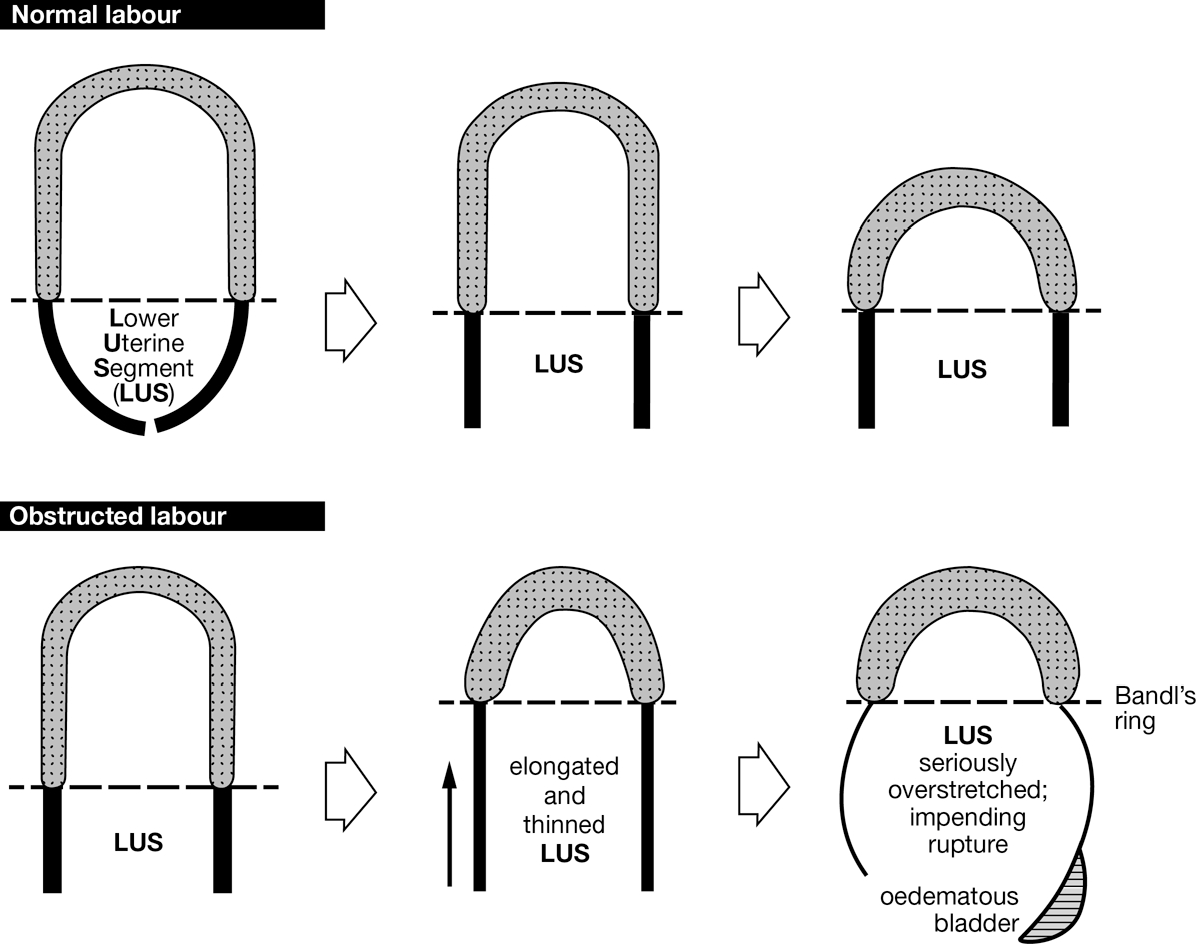
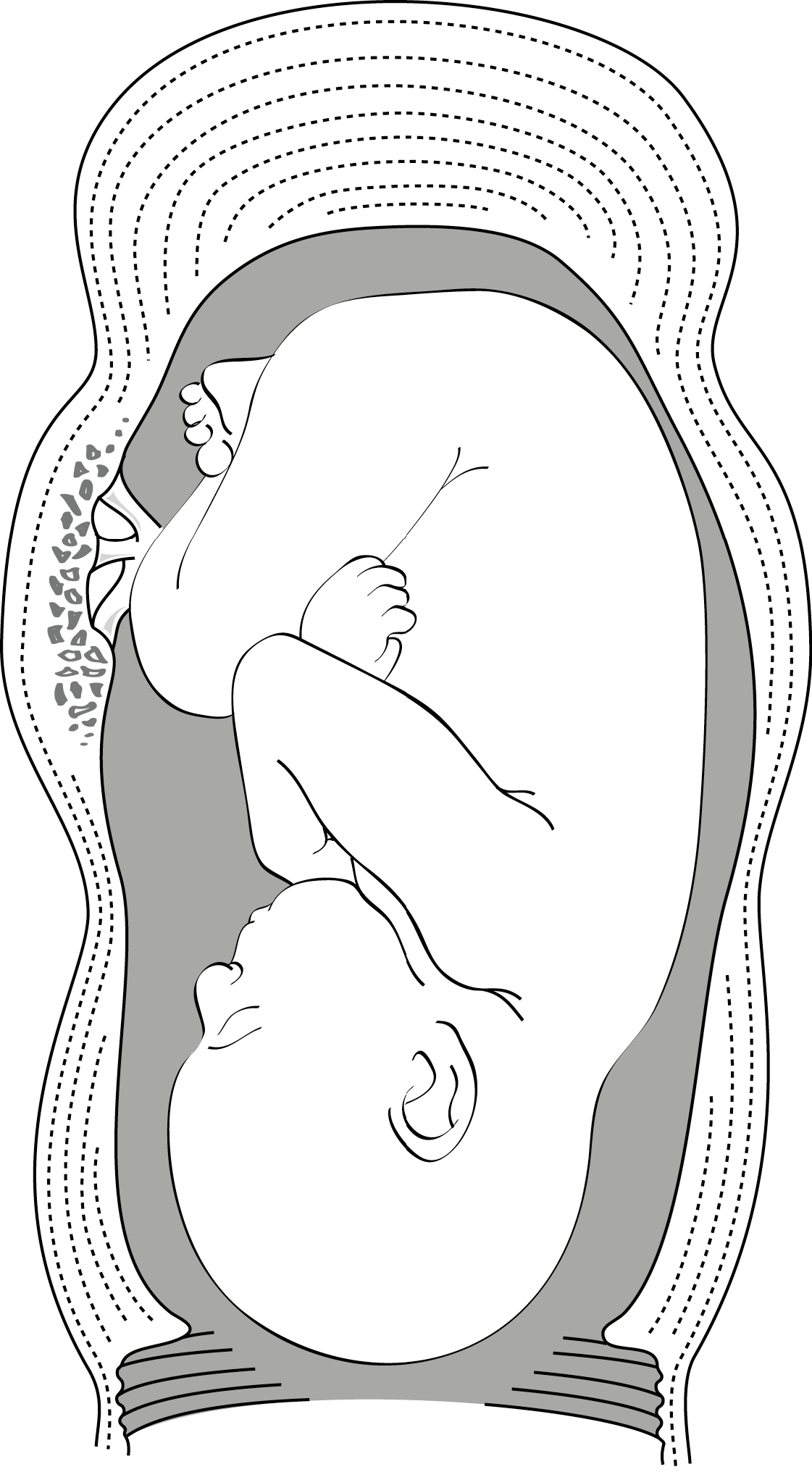
- often, Bandl’s ring (Figures 3.3 and 3.4), a sign of obstructed labour. At first glance the Bandl’s ring may look like a distended bladder.
Figure 3.3 - Mechanism of Bandl’s ring formationaCitation a.Adapted from Primary Surgery Vol.1 – Non-Trauma: The surgery of labour. German Society of Tropical Surgery.
http://www.primary-surgery.org/ps/vol1/html/sect0016.html
Figure 3.4 - Impending rupture: hourglass uterus “Bandl's ring”
- Rupture:
- shoulder-tip pain or increased pain on inspiration, a sign of haemoperitoneum. Sometimes the pain is sudden, during a contraction, and the patient describes a “tearing” sensation. The pain may be less obvious in cases of posterior uterine rupture.
- hypovolaemic shock due to bleeding (rapid or weak or unmeasurable pulse, very low or undetectable blood pressure, tachypnoea, cold sensation, damp skin, agitation or anxiety).
- contractions stop.
- slow foetal heart rate or no heart tones.
- sometimes feels like foetus can be palpated just below the skin if large, complete rupture. Foetus is usually dead.
After delivery
A rupture may be discovered during a haemorrhage: uterine exploration after delivery of the placenta reveals the rupture.
3.3.3 Management
See also algorithm.
- Insert 2 IV lines (16-18G catheter) and administer Ringer lactate.
- Measure heart rate and blood pressure; assess the severity of the bleeding.
- Insert a Foley urinary catheter.
- Emergency laparotomy with rapid caesarean section, fluid replacement and, in most cases, blood transfusion.
- Depending on the type of rupture, the patient’s condition, the time between rupture and laparotomy and whether there are signs of infection, suture the uterus or perform hysterectomy.
Keep the surgery as brief as possible, as these patients are often in poor general condition (anaemic, in particular).
A sub-umbilical midline incision is preferable (better exposure), sometimes with peri-umbilical extension.
The tear is usually in the lower segment, anterior and low. Enlarge the tear to allow extraction of the foetus.
Check the integrity of the bladder, which may have been injured if it is very adherent to the lower uterine segment (continuous suture in one or two planes and urinary catheterisation for at least 7 days).
Attempt repair whenever possible. Before suturing the uterine muscle, trim ragged, bruised edges.
In the event of uterine infection or extensive rupture with severe bruising around the wound or suture repair is not possible, perform a subtotal hysterectomy with ovarian conservation.
Given the risk of another uterine rupture during subsequent pregnancies, bilateral tubal ligation may be advised or indicated. This is best discussed before surgery. The patient’s consent is required.
- (a)Adapted from Primary Surgery Vol.1 – Non-Trauma: The surgery of labour. German Society of Tropical Surgery.
http://www.primary-surgery.org/ps/vol1/html/sect0016.html