On this page
Uterus turns inside-out, typically as the placenta is delivered. Usually due to uterine atony (grand multiparity) or forceful traction on the cord.
8.4.1 Diagnosis
- Usually, intense pelvic pain with feeling of “something coming down” and haemorrhage of variable severity, quickly followed by hypovolaemic shock.
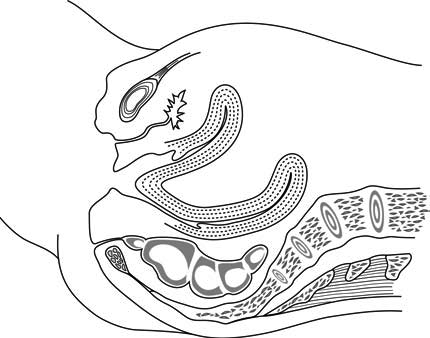
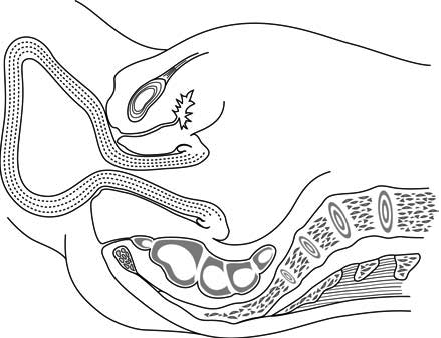
- Uterine fundus not apparent on abdominal palpation, protrudes into the vagina, or protrudes from the vaginal opening (Figures 8.5 and 8.6).
Figure 8.5 - The inverted uterus does not reach the vaginal opening
Figure 8.6 - The uterus is totally inverted and protrudes through the vaginal opening
8.4.2 Management
- Treat the shock and the haemorrhage immediately: see Resuscitation, Table 8.1. Blood transfusion in the event of immediate massive haemorrhage.
- Administer tranexamic acid IV (Section 8.2.1) in the event of massive haemorrhage or if bleeding persists after 15 minutes of initial management.
- Trendelenburg position (dorsal decubitus, head down).
- Insert a Foley catheter and monitor urine output.
- Perform general anaesthesia if possible.
- If uterotonic treatment is in progress, stop it long enough to reduce the inversion.
- Swab the perineum with 10% povidone iodine.
- If the placenta has not detached, do not perform manual removal until after reducing the inversion.
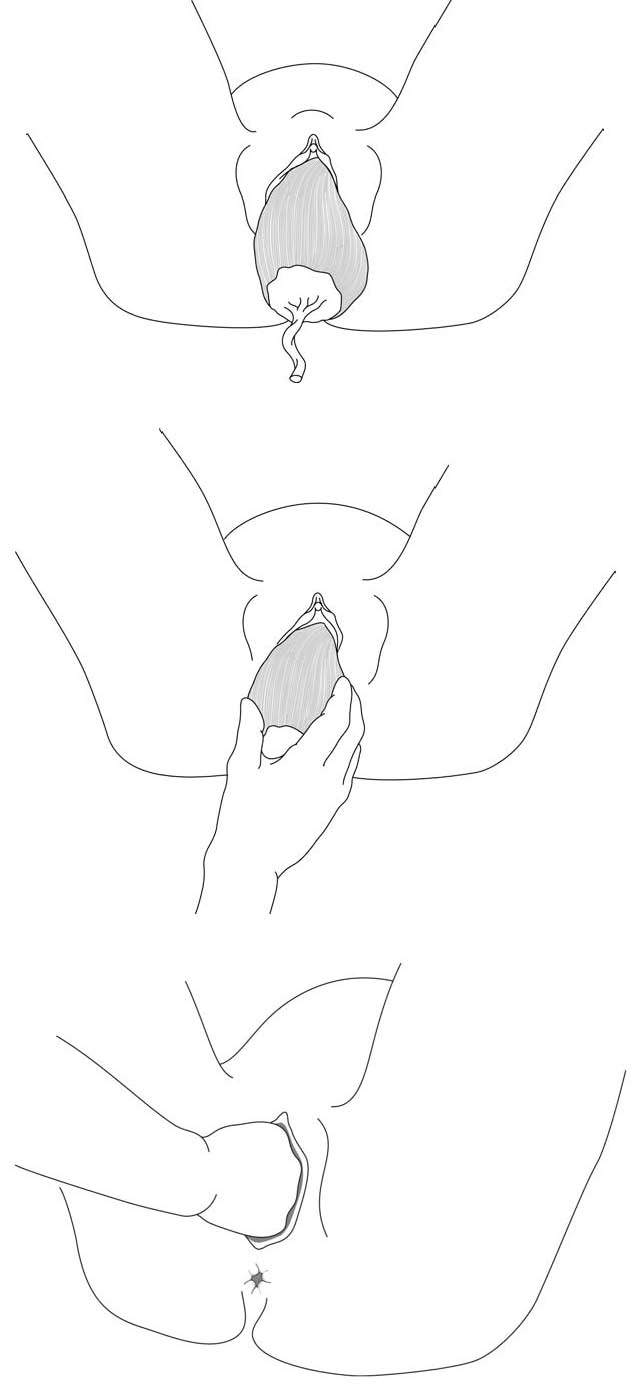
- While compressing the uterus, push it gradually back through the cervix with one hand (Figures 8.7), toward the umbilicus, to return it to its normal position. Use the other hand, placed on the abdomen, to hold the uterus in place.
- If necessary, explore the uterus (gently, to avoid recurrence) in order to remove any clots.
- Give routine antibiotic prophylaxis (Chapter 9, Section 9.1.2).
- Resume or start uterotonic treatment: oxytocin slow IV or IM: 5 or 10 IU (or, if not available, methylergometrine IM: 0.2 mg or misoprostol sublingually: 800 micrograms).
Figure 8.7 - Manual reduction of the inverted uterus
If manual reduction of the uterus fails, consider abdominal surgery: reduction of the inversion with possible section of the retracted oedematous cervix, or even delayed hysterectomy after necrosis develops.