Early postpartum haemorrhage is defined as bleeding that occurs within 24 hours (usually immediately) after delivery of the placenta. The volume exceeds the normal 500 ml third stage blood loss.
Close delivery room monitoring is crucial for 2 hours post-partum, in order to rapidly identify and treat postpartum haemorrhage (PPH).
Blood loss is often underestimated (up to 50%).
Delay in treatment can lead to coagulation disorders, with a risk of massive, diffuse bleeding.
The four main causes of PPH are:
- Uterine atony (70% of cases): the placenta has been expelled, but the uterus fails to retract. The uterus gets larger, extends, and becomes soft. Factors for uterine atony include: overstretching (polyhydramnios, multiple pregnancy, foetal macrosomia), prolonged labour and infection (chorioamniotitis). It can be the cause or an aggravating factor of the PPH.
- Obstetric trauma (20% of cases): uterine rupture, particularly in case of vaginal delivery in women with a scarred uterus but also in women without uterine scarring; cervical and vaginal lacerations; uterine inversion.
- Retained placenta (10% of cases): the entire placenta or a fragment of the placenta remains in the uterus.
- Coagulation disorders (< 1% of cases): see Chapter 3, Section 3.2.2.
8.2.1 Management during the first 30 minutes
- Ask for help as resuscitation measures and obstetric management must be performed in parallel.
- Record in a chart: results of the initial evaluation, monitoring and actions, indicating the times.
Table 8.1 - Initial management
|
Resuscitation |
Initial obstetric management |
|---|---|
Objectives: systolic BP ≥ 90 mmHg, SpO2 ≥ 95%, normal level of consciousness, urine output ≥ 30 ml/hour.
|
misoprostol sublingually
(b)Citation b.If the sublingual route is not feasible, administer the same dose rectally.
: 800 micrograms
[1]Citation 1.World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva, 2012. |
8.2.2 Management of persistent haemorrhage
Table 8.2 - Management after the first 30 minutes
|
Resuscitation |
Further obstetric management |
|---|---|
|
|
8.2.3 Management of immediate massive haemorrhage
In the event of 150 ml of blood loss per minute or shock:
- Perform initial management as quickly as possible and do not wait 30 minutes to perform further obstetric management (intrauterine balloon tamponade, surgical procedures).
- Start transfusion as quickly as possible.
- If necessary, perform one of the additional compression measures below.
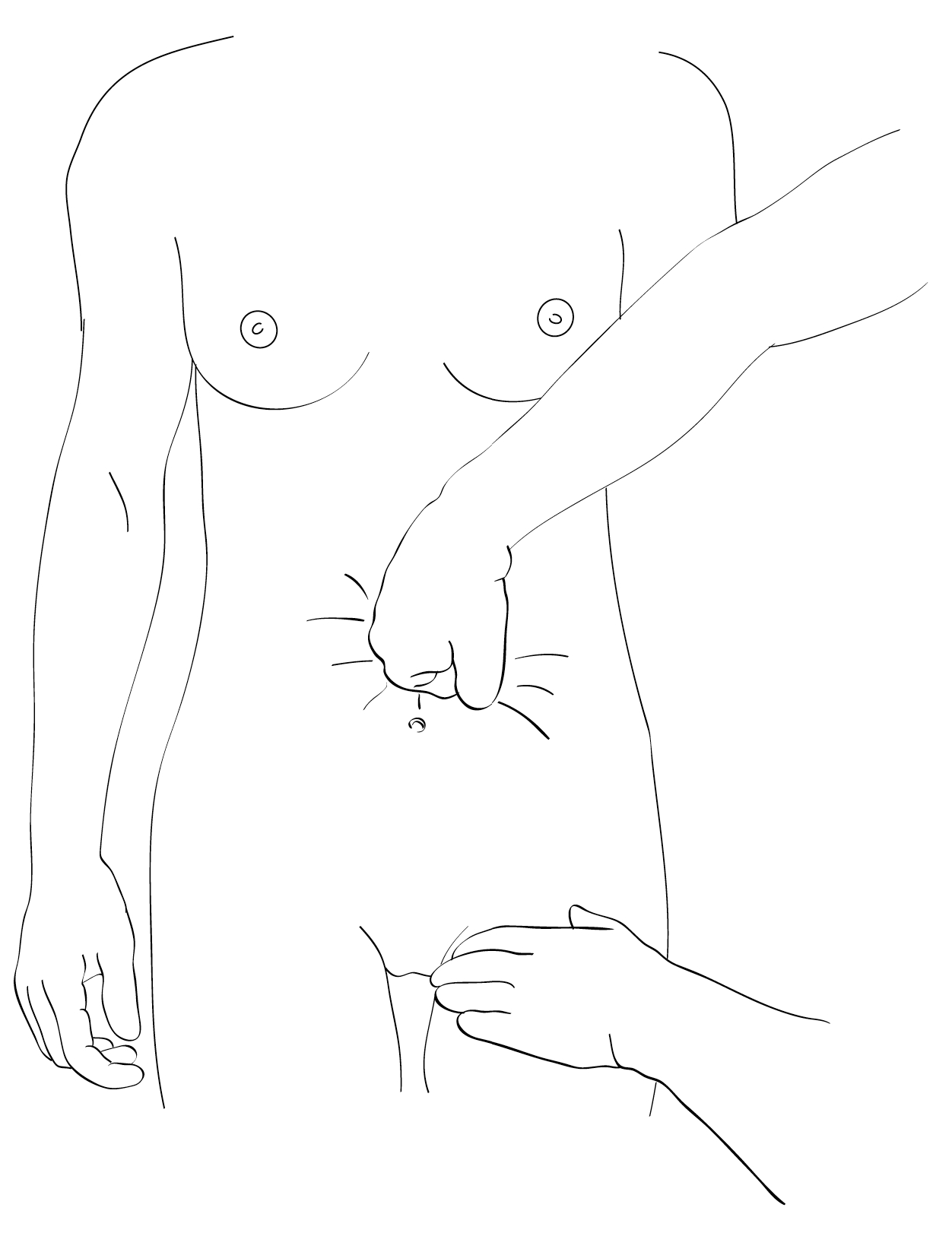
Aortic compression
Apply pressure to the abdominal aorta (just above the umbilicus) until the femoral pulse is no longer palpable, for example, the time it takes to insert an intrauterine balloon or start laparotomy (Figure 8.2).
Figure 8.2 - Aortic compression
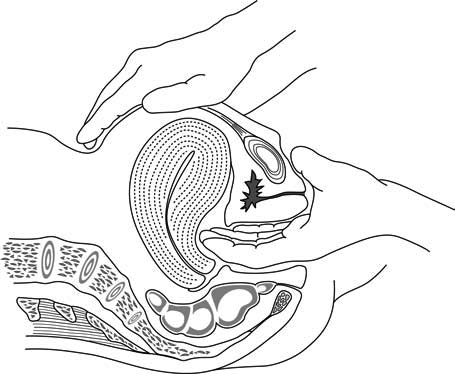
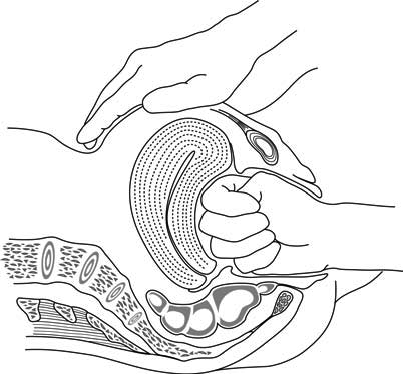
Bimanual uterine compression (Figure 8.3 and Figure 8.4).
Figure 8.3 - Uterine compression between fingers in the vagina and a hand on the abdomen
Figure 8.4 - Uterine compression between the fist and a hand on the abdomen
8.2.4 Cause-specific management
If the following causes are identified, additional specific management is required.
Obstetric trauma
- Uterine rupture: Chapter 3, Section 3.3.
- Cervical or vaginal tears: Section 8.5.
- An episiotomy can bleed: temporarily stop arterial bleeding with a clamp and suture as quickly as possible.
- Uterine inversion: Section 8.4.
Retained placenta
- Immediate manual removal if the placenta has not yet delivered and/or routine uterine exploration to remove any clots or placental debris (allows good uterine retraction) and to verify that there was no uterine rupture (for vaginal deliveries with a scarred uterus, in particular).
- Perform manual placenta removal and manual uterine exploration under anaesthesia. Do not proceed without anaesthesia unless anaesthesia cannot be performed immediately.
- Give routine antibiotic prophylaxis (Chapter 9, Section 9.1.2).
- In rare cases, it is impossible to remove the placenta manually because there is no cleavage plane between the placenta and the uterine wall (placenta accreta). In this event, refer for hysterectomy.
Coagulation disorders
- In the event of coagulation disorders, transfuse:
- fresh whole blood (blood freshly collected, for less than 4 hours, and that has not been refrigerated), or
- packed red blood cells or whole blood + fresh frozen plasma.
- Coagulation disorders may be the cause and the result of PPH. Active management of PPH reduces the risk of secondary coagulation disorders.
- (a)For more information on B-Lynch suture: A Comprehensive Textbook of Postpartum Hemorrhage 2nd Edition. Section 9, Chapter 51: Therapy for Non-atonic Bleeding, C. B-Lynch and H. Shah. Conservative Surgical Management.
http://www.glowm.com/pdf/PPH_2nd_edn_Chap-51.pdf
- aIf transfusion is performed, the blood must have been tested (HIV-1, HIV-2, hepatitis B, hepatitis C and syphilis, and malaria in endemic areas).
- bIf the sublingual route is not feasible, administer the same dose rectally.
- cIf an intrauterine balloon is inserted in a BEmONC facility, it is imperative to transfer the patient to a CEmONC facility in order to have surgical resources on hand should they be necessary.
- 1.World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva, 2012.
http://apps.who.int/iris/bitstream/10665/75411/1/9789241548502_eng.pdf