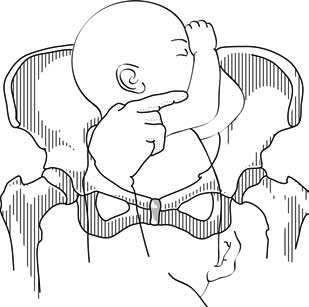
Presentation of the feet or buttocks of the foetus.
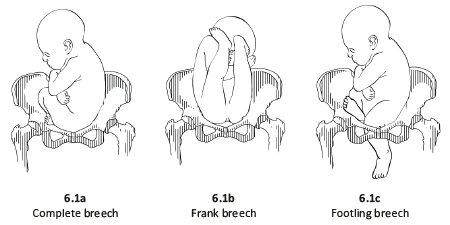
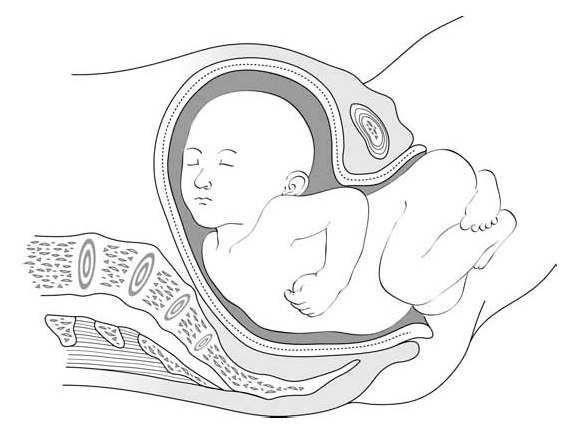
6.1.1 The different breech presentations
- In a complete breech presentation, the legs are tucked, and the foetus is in a crouching position (Figure 6.1a).
- In a frank breech presentation, the legs are extended, raised in front of the torso, with the feet near the head (Figure 6.1b).
- In a footling breech presentation (rare), one or both feet present first, with the buttocks higher up and the lower limbs extended or half-bent (Figure 6.1c).
Figures 6.1 - Breech presentations
6.1.2 Diagnosis
- The cephalic pole is palpable in the uterine fundus; round, hard, and mobile; the indentation of the neck can be felt.
- The inferior pole is voluminous, irregular, less hard, and less mobile than the head.
- During labour, vaginal examination reveals a “soft mass” divided by the cleft between the buttocks, with a hard projection at end of the cleft (the coccyx and sacrum).
- After rupture of the membranes: the anus can be felt in the middle of the cleft; a foot may also be felt.
- The clinical diagnosis may be difficult: a hand may be mistaken for a foot, a face for a breech.
6.1.3 Management
Route of delivery
Before labour, external version (Chapter 7, Section 7.7) may be attempted to avoid breech delivery.
If external version is contra-indicated or unsuccessful, the breech position alone – in the absence of any other anomaly – is not, strictly speaking, a dystocic presentation, and does not automatically require a caesarean section. Deliver vaginally, if possible – even if the woman is primiparous.
Breech deliveries must be done in a CEmONC facility, especially for primiparous women.
Favourable factors for vaginal delivery are:
- Frank breech presentation;
- A history of vaginal delivery (whatever the presentation);
- Normally progressing dilation during labour.
The footling breech presentation is a very unfavourable position for vaginal delivery (risk of foot or cord prolapse). In this situation, the route of delivery depends on the number of previous births, the state of the membranes and how far advanced the labour is.
During labour
- Monitor dilation every 2 to 4 hours.
- If contractions are of good quality, dilation is progressing, and the foetal heart rate is regular, an expectant approach is best. Do not rupture the membranes unless dilation stops.
- If the uterine contractions are inadequate, labour can be actively managed with oxytocin.
Note: if the dilation stales, transfer the mother to a CEmONC facility unless already done, to ensure access to surgical facility for potential caesarean section.
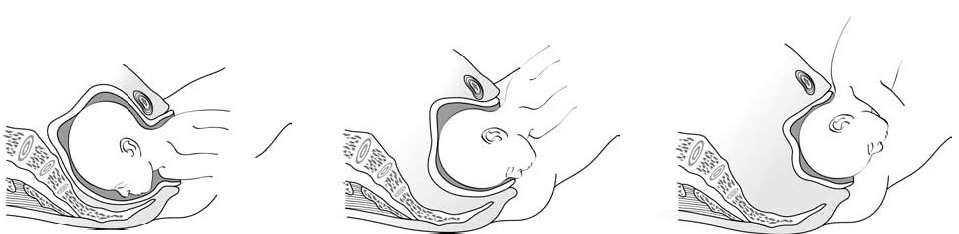
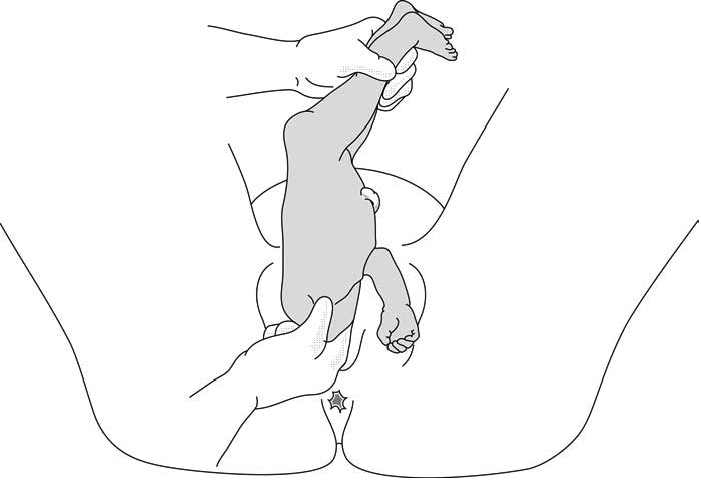
At delivery
- Insert an IV line before expulsion starts.
- Consider episiotomy at expulsion. Episiotomy is performed when the perineum is sufficiently distended by the foetus's buttocks.
- Presence of meconium or meconium-stained amniotic fluid is common during breech delivery and is not necessarily a sign of foetal distress.
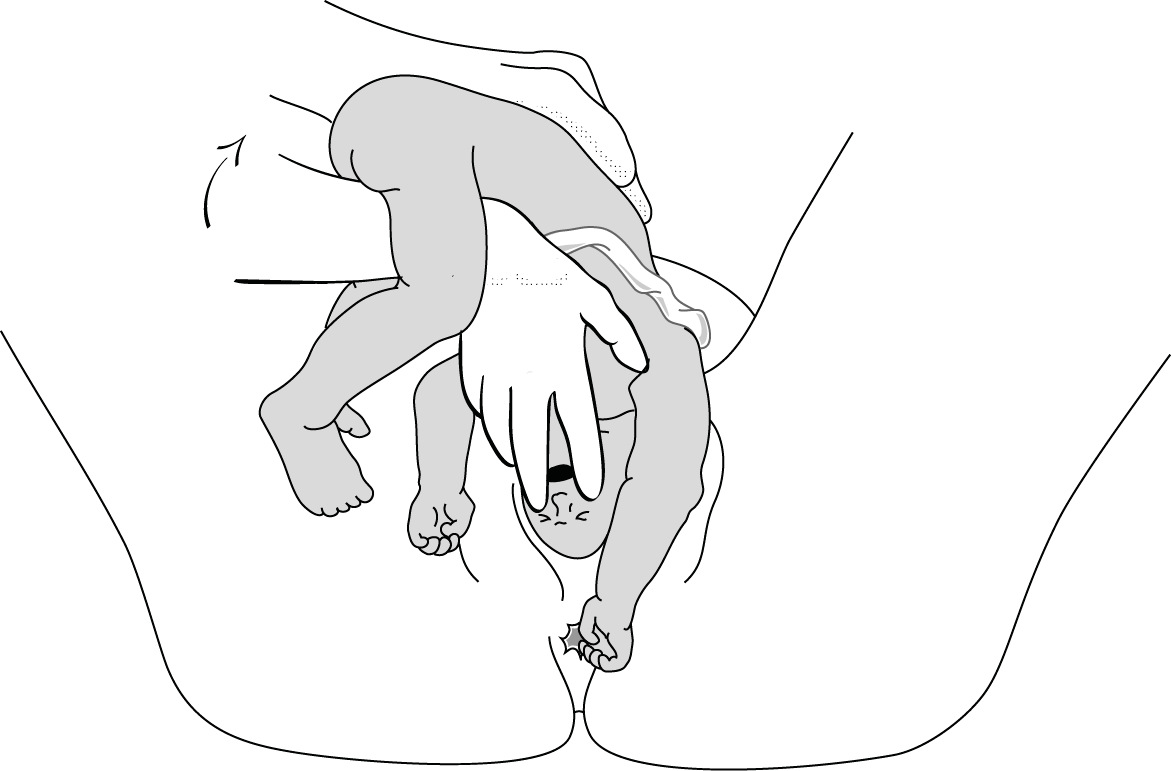
- The infant delivers unaided, as a result of the mother's pushing, simply supported by the birth attendant who gently holds the infant by the bony parts (hips and sacrum), with no traction. Do not pull on the legs.
Once the umbilicus is out, the rest of the delivery must be completed within 3 minutes, otherwise compression of the cord will deprive the infant of oxygen.
Do not touch the infant until the shoulder blades appear to avoid triggering the respiratory reflex before the head is delivered.
- Monitor the position of the infant's back; impede rotation into posterior position.
Figures 6.2 - Breech delivery
 |
 |
|
|
6.1.4 Breech delivery problems
Posterior orientation
If the infant’s back is posterior during expulsion, take hold of the hips and turn into an anterior position (this is a rare occurrence).
Obstructed shoulders
The shoulders can become stuck and hold back the infant's upper chest and head. This can occur when the arms are raised as the shoulders pass through the mother's pelvis. There are 2 methods for lowering the arms so that the shoulders can descend:
1 - Lovset's manoeuvre
- With thumbs on the infant's sacrum, take hold of the hips and pelvis with the other fingers.
- Turn the infant 90° (back to the left or to the right), to bring the anterior shoulder underneath the symphysis and engage the arm. Deliver the anterior arm.
- Then do a 180° counter-rotation (back to the right or to the left); this engages the posterior arm, which is then delivered.
Figures 6.3 - Lovset's manoeuvre
6.3a - Turning the infant to bring down the anterior shoulder
6.3b - Downward traction and descent of shoulders along the midline (sacral-pubic) axis
6.3c - Delivering the anterior arm and shoulder
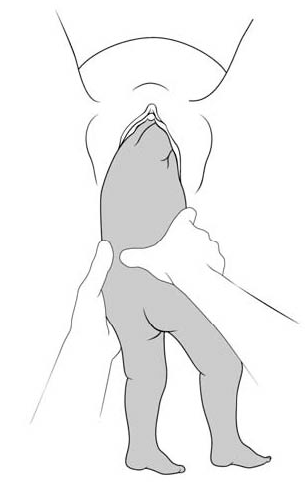
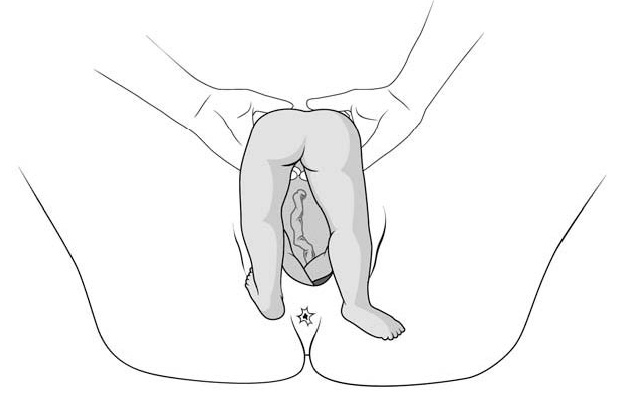
2 - Suzor’s manoeuvre
In case the previous method fails:
- Turn the infant 90° (its back to the right or to the left).
- Pull the infant downward: insert one hand along the back to look for the anterior arm. With the operator thumb in the infant armpit and middle finger along the arm, bring down the arm (Figure 6.4a).
- Lift infant upward by the feet in order to deliver the posterior shoulder (Figure 6.4b).
Figures 6.4 - Suzor's manoeuvre
6.4a - Bringing down the anterior arm
6.4b - Delivering the posterior shoulder
Head entrapment
The infant's head is bulkier than the body, and can get trapped in the mother's pelvis or soft tissue.
There are various manoeuvres for delivering the head by flexing it, so that it descends properly, and then pivoting it up and around the mother's symphysis. These manoeuvres must be done without delay, since the infant must be allowed to breathe as soon as possible. All these manoeuvres must be performed smoothly, without traction on the infant.
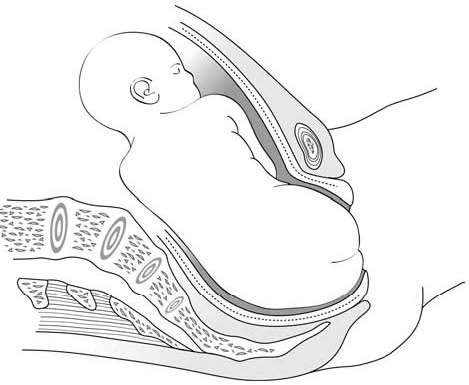
1 - Bracht's manoeuvre
- After the arms are delivered, the infant is grasped by the hips and lifted with two hands toward the mother's stomach, without any traction, the neck pivoting around the symphysis.
- Having an assistant apply suprapubic pressure facilitates delivery of the aftercoming head.
Figures 6.5 - Bracht's manoeuvre
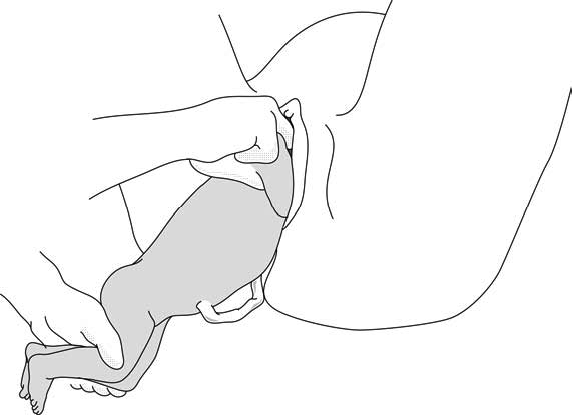
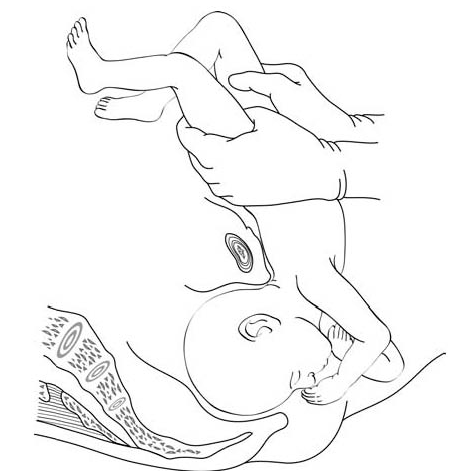
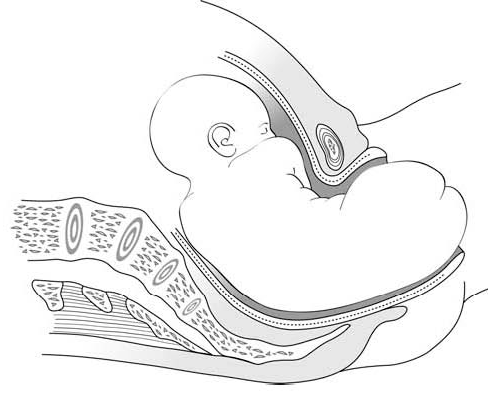
2 - Modified Mauriceau manoeuvre
In case the previous method fails:
- Infant's head occiput anterior.
- Kneel to get a good traction angle: 45° downward.
- Support the infant on the hand and forearm, then insert the index and middle fingers, placing them on the infant’s maxilla. Placing the index and middle fingers into the infant’s mouth is not recommended, as this can fracture the mandible.
- Place the index and middle fingers of the other hand on either side of the infant's neck and lower the infant's head to bring the sub-occiput under the symphysis (Figure 6.6a).
- Tip the infant’s head and with a sweeping motion bring the back up toward the mother's abdomen, pivoting the occiput around her symphysis pubis (Figure 6.6b).
- Suprapubic pressure on the infant's head along the pelvic axis helps delivery of the head.
- As a last resort, symphysiotomy (Chapter 5, Section 5.7) can be combined with this manoeuvre.
Figures 6.6 - Modified Mauriceau manoeuvre
6.6a - Step 1
Infant straddles the birth attendant's forearm; the head, occiput anterior, is lowered to bring the occiput in contact with the symphysis.
6.6b - Step 2
The infant's back is tipped up toward the mother's abdomen.
3 - Forceps on aftercoming head
This procedure can only be performed by an operator experienced in using forceps.