Pain results from a variety of pathological processes. It is expressed differently by each patient depending on cultural background, age, etc. It is a subjective experience meaning that only the individual is able to assess his/her level of pain. Regular assessment of the intensity of pain is indispensable in establishing effective treatment.
Clinical features
Pain assessment
- Intensity: use a simple verbal scale in children over 5 years and adults, and NFCS or FLACC scales in children less than 5 years (see Pain evaluation scales).
- Pattern: sudden, intermittent, chronic; at rest, at night, on movement, during care procedures, etc.
- Character: burning, cramping, spasmodic, radiating, etc.
- Aggravating or relieving factors, etc.
Clinical examination
- Of the organ or area where the pain is located.
- Specific signs of underlying disease (e.g. bone or osteoarticular pain may be caused by a vitamin C deficiency) and review of all systems.
- Associated signs (fever, weight loss, etc.).
Synthesis
The synthesis of information gathered during history taking and clinical examination allows aetiological diagnosis and orients treatment. It is important to distinguish:
- Nociceptive pain: it presents most often as acute pain and the cause-effect relationship is usually obvious (e.g. acute post-operative pain, burns, trauma, renal colic, etc.). The pain may be present in different forms, but neurological exam is normal. Treatment is relatively well standardized.
- Neuropathic pain, due to a nerve lesion (section, stretching, ischaemia): most often chronic pain. On a background of constant, more or less localized pain, such as paraesthesia or burning, there are recurrent acute attacks such as electric shock-like pain, frequently associated with disordered sensation (anaesthesia, hypo or hyperaesthesia). This type of pain is linked to viral infections directly affecting the CNS (herpes simplex, herpes zoster), neural compression by tumors, post- amputation pain, paraplegia, etc.
- Mixed pain (cancer, HIV) for which management requires a broader approach.
Pain evaluation scales
Self-evaluation scale - Children over 5 years and adults
Simple verbal scale (SVS)
Intensity | No | Mild | Moderate | Severe pain |
|---|---|---|---|---|
Scoring | 0 | 1 | 2 | 3 |
Write down | 0 | + | ++ | +++ |
Observational evaluation scale - Children 2 months-5 years
FLACC scale (Face Limb Activity Cry Consolability)
Items | Scoring | ||
|---|---|---|---|
| 0 | 1 | 2 | |
Face | No particular expression or smile | Occasional grimace or frown, withdrawn, disinterested | Frequent to constant frown, clenched jaw, quivering chin |
Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking, or legs drawn up |
Activity | Lying quietly, normal position, moves easily | Squirming, shifting back and forth, tense | Arched, rigid or jerking |
Cry | No cry (awake or asleep) | Moans or whimpers, occasional complaint | Crying steadily, screams or sobs, frequent complaints |
Consolability | Content, relaxed | Reassured by occasional touching, hugging or being talked to, distractible | Difficult to console or comfort |
Each category is scored from 0 to 2, giving a final score between 0 and 10.
0 to 3: mild pain, 4 to 7: moderate pain, 7 to 10: severe pain
Observational evaluation scale - Children under 2 months
NFCS scale (Neonatal Facial Coding System)
Items | Scoring | 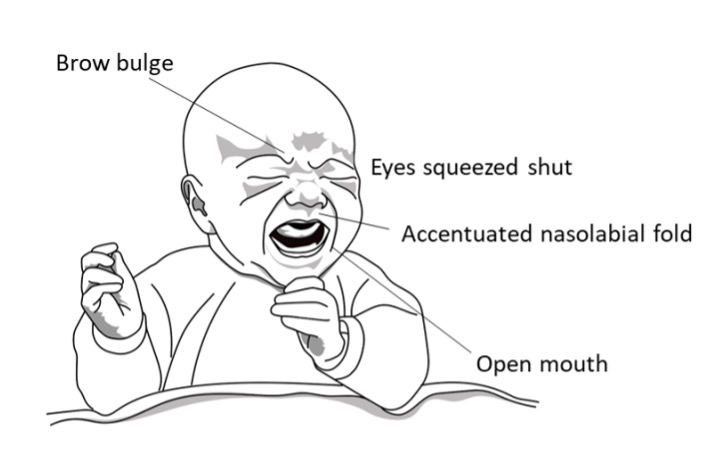
| |
| 0 | 1 | ||
| Brow bulge | no | yes | |
| Eye squeeze | no | yes | |
| Nasolabial furrow | no | yes | |
| Open lips | no | yes | |
A score of 2 or more signifies significant pain, requiring analgesic treatment.
Treatment
Treatment depends on the type and intensity of the pain. It may be both aetiological and symptomatic if a treatable cause is identified. Treatment is symptomatic only in other cases (no cause found, non-curable disease).
Nociceptive pain
The WHO classifies analgesics used for this type of pain on a three-step ladder:
- Step 1: non-opioid analgesics such as paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs).
- Step 2: weak opioid analgesics such as codeine and tramadol. Their combination with one or two Step 1 analgesics is recommended.
- Step 3: strong opioid analgesics, first and foremost morphine. Their combination with one or two Step 1 analgesics is recommended.
The treatment of pain is based on a few fundamental concepts:
- Pain can only be treated correctly if it is correctly evaluated. The only person who can evaluate the intensity of pain is the patient himself. The use of pain assessment scales is invaluable.
- The pain evaluation observations should be recorded in the patient chart in the same fashion as other vital signs.
- Treatment of pain should be as prompt as possible.
- It is recommended to administer analgesics in advance when appropriate (e.g. before painful care procedures).
- Analgesics should be prescribed and administered at fixed time intervals (not on demand).
- Oral forms should be used whenever possible.
- The combination of different analgesic drugs (multimodal analgesia) is advantageous.
- Start with an analgesic from the level presumed most effective: e.g., in the event of a fractured femur, start with a Step 3 analgesic.
- The treatment and dose chosen are guided by the assessment of pain intensity, but also by the patient’s response which may vary significantly from one person to another.
Treatment of acute pain
Mild pain | Paracetamol + /- NSAID |
Moderate pain | Paracetamol + /- NSAID + tramadol or codeine |
Severe pain | Paracetamol + /- NSAID + morphine |
| Analgesics | Children | Adults (except pregnant/breast-feeding women) | Remarks |
|---|---|---|---|---|
Level 1 | paracetamol PO | < 1 month: 10 mg/kg every 6 to 8 hours (max. 40 mg/kg daily) ≥ 1 month: 15 mg/kg every 6 to 8 hours (max. 60 mg/kg daily)
| 1 g every 6 to 8 hours (max. 4 g daily) | The efficacy of IV paracetamol is not superior to the efficacy of oral paracetamol; the IV route is restricted to situations where oral administration is impossible. |
paracetamol IV | < 1 month: 7.5 mg/kg every 6 hours (max. 30 mg/kg daily) ≥ 1 month and < 10 kg: 10 mg/kg every 6 hours (max. 30 mg/kg daily) ≥ 10 kg: 15 mg/kg every 6 hours (max. 60 mg/kg daily) | < 50 kg: 15 mg/kg every 6 hours (max. 60 mg/kg daily) ≥ 50 kg: 1 g every 6 hours (max. 4 g daily) | ||
acetylsalicylic acid (aspirin) PO | – | 300 mg to 1 g every 4 to 6 hours (max. 4 g daily) | Avoid in children less than 16 years. | |
diclofenac IM | – | 75 mg once daily | Treatment must be as short as possible. | |
ibuprofen PO | > 3 months: 5 to 10 mg/kg every 6 to 8 hours (max. 30 mg/kg daily) > 12 years: as for adults | 200 to 400 mg every 6 to 8 hours (max. 1200 mg daily) | ||
Level 2
| codeine PO | > 12 years: 30 to 60 mg every 4 to 6 hours (max. 240 mg daily) | 30 to 60 mg every 4 to 6 hours (max. 240 mg daily) | Add a laxative if treatment > 48 hours. |
tramadol PO | > 12 years: 50 to 100 mg every 4 to 6 hours (max. 400 mg daily) | 50 to 100 mg every 4 to 6 hours (max. 400 mg daily) |
25 to 50 mg every 12 hours in elderly patients and in patients with severe renal or hepatic impairment.
| |
tramadol IM, slow IV or infusion | > 12 years: 50 to 100 mg every 4 to 6 hours (max. 600 mg daily) | 50 to 100 mg every 4 to 6 hours (max. 600 mg daily) | ||
Level 3 | morphine PO immediate release (MIR) | > 6 months: 0.15 mg/kg every 4 hours, to be ajusted in relation to pain intensity | 10 mg every 4 hours, to be ajusted in relation to pain intensity | • Reduce the dose by half in elderly patients and patients with renal or hepatic impairment. • Add a laxative if treatment > 48 hours. |
morphine PO sustained release (MSR) | The daily dose is determined during the initial treatment with immediate release morphine (MIR). If treatment is initiated directly with MSR: | The daily dose is determined during the initial treatment with immediate release morphine (MIR). If treatment is initiated directly with MSR: | • Do not initiate treatment with the MSR in elderly patients and patients with renal or hepatic impairment. Begin treatment with MIR. • Add a laxative if treatment > 48 hours. | |
morphine SC, IM | > 6 months: 0.1 to 0.2 mg/kg every 4 hours | 0.1 to 0.2 mg/kg every 4 hours | • Reduce doses by half and administer less frequently, according to clinical response, in elderly patients and patients with severe renal or hepatic impairment. • Add a laxative if treatment > 48 hours. | |
morphine IV | > 6 months: 0.1 mg/kg administered in fractionated doses (0.05 mg/kg every 10 minutes) every 4 hours if necessary | 0.1 mg/kg administered in fractionated doses (0.05 mg/kg every 10 minutes) every 4 hours if necessary |
Notes on the use of morphine and derivatives:
- Morphine is an effective treatment for many types of severe pain. Its analgesic effect is dosedependent. Its adverse effects have often been exaggerated and should not be an obstacle to its use.
- The most serious adverse effect of morphine is respiratory depression, which may be fatal. This adverse effect results from overdose. It is, therefore, important to increase doses gradually. Respiratory depression is preceded by drowsiness, which is a warning to monitor respiratory rate (RR).
The RR should remain equal to or greater than the thresholds indicated below:
Children 1 to 12 months | RR ≥ 25 respirations/minute |
Children 1 to 2 years | RR ≥ 20 respirations/minute |
Children 2 to 5 years | RR ≥ 15 respirations/minute |
Children > 5 years and adults | RR ≥ 10 respirations/minute |
Respiratory depression must be identified and treated quickly: verbal and physical stimulation of the patient; administration of oxygen; respiratory support (bag and mask) if necessary. If no improvement, administer naloxone (antagonist of morphine) in bolus to be repeated every minute until RR normalises and the excessive drowsiness resolves: 5 micrograms/kg in children and 1 to 3 micrograms/kg in adults.
- Morphine and codeine always cause constipation. A laxative should be prescribed if the opioid treatment continues more than 48 hours. Lactulose PO is the drug of choice: children < 1 year: 5 ml daily; children 1-6 years: 5 to 10 ml daily; children 7-14 years: 10 to 15 ml daily; adults: 15 to 45 ml daily.
If the patient’s stools are soft, a stimulant laxative (bisacodyl PO: children > 3 years: 5 to 10 mg once daily; adults: 10 to 15 mg once daily) is preferred.
Nausea and vomiting are common at the beginning of treatment.
Children:
ondansetron PO: 0.15 mg/kg (max. 4 mg per dose) up to 3 times daily
Do not use metoclopramide in children.
Adults:
haloperidol PO (2 mg/ml oral solution): 1 to 2 mg up to 6 times daily or metoclopramide PO: 5 to 10 mg 3 times daily with an interval of at least 6 hours between each dose
Do not combine haloperidol and metoclopramide.
- For chronic pain in late stage disease (cancer, AIDS etc.), morphine PO is the drug of choice. It may be necessary to increase doses over time according to pain assessment. Do not hesitate to give sufficient and effective doses.
- Morphine, tramadol and codeine have similar modes of action and should not be combined.
- Buprenorphine, nalbuphine and pentazocine must not be combined with morphine, pethidine, tramadol or codeine because they have competitive action.
Treatment of nociceptive pain in pregnant and breast-feeding women
Analgesics | Pregnancy | Breast-feeding | ||
|---|---|---|---|---|
| 0-5 months | From 6th month | |||
| paracetamol | first choice | first choice | first choice |
aspirin | avoid | contra-indicated | avoid | |
ibuprofen | avoid | contra-indicated | possible | |
| codeine | possible | The neonate may develop withdrawal symptoms, respiratory depression and drowsiness in the event of prolonged administration of large doses at the end of the thirdtrimester. Closely monitor the neonate. | Use with caution, for a short period (2-3 days), at the lowest effective dose. Monitor the mother and the child: in the event of excessive drowsiness, stop treatment. |
| tramadol | possible | The child may develop drowsiness when the mother receives tramadol at the end of the thirdtrimester and during breast-feeding. Administer with caution, for a short period, at the lowest effective dose, and monitor the child. | ||
Level 3 | morphine | possible | The child may develop withdrawal symptoms, respiratory depression and drowsiness when the mother receives morphine at the end of the third trimester and during breast-feeding. Administer with caution, for a short period, at the lowest effective dose, and monitor the child. | |
Neuropathic pain
Commonly used analgesics are often ineffective in treating this type of pain.
Treatment of neuropathic pain is based on a combination of two centrally acting drugs:
amitriptyline PO
Adults: 25 mg once daily at bedtime (Week 1); 50 mg once daily at bedtime (Week 2); 75 mg once daily at bedtime (as of Week 3); max.150 mg daily. Reduce the dose by half in elderly patients.
carbamazepine PO
Adults: 200 mg once daily at bedtime (Week 1); 200 mg 2 times daily (Week 2); 200 mg 3 times daily (as of Week 3)
Given its teratogenic risk, carbamazepine should only be used in women of childbearing age when covered by effective contraception (intrauterine device or injectable progestogen). It is not recommended in pregnant women.
Mixed pain
In mixed pain with a significant component of nociceptive pain, such as in cancer or AIDS, morphine is combined with antidepressants and antiepileptics.
Chronic pain
In contrast to acute pain, medical treatment alone is not always sufficient in controlling chronic pain. A multidisciplinary approach including medical treatment, physiotherapy, psychotherapy and nursing is often necessary to allow good pain relief and encourage patient selfmanagement.
Co-analgesics
The combination of certain drugs may be useful or even essential in the treatment of pain: antispasmodics, muscle relaxants, anxiolytics, corticosteroids, local anaesthesia, etc.