Last updated: August 2022
Urethral discharge is seen almost exclusively in men. The principal causative organisms are Neisseria gonorrhoeae (gonorrhoea) and Chlamydia trachomatis (chlamydia).
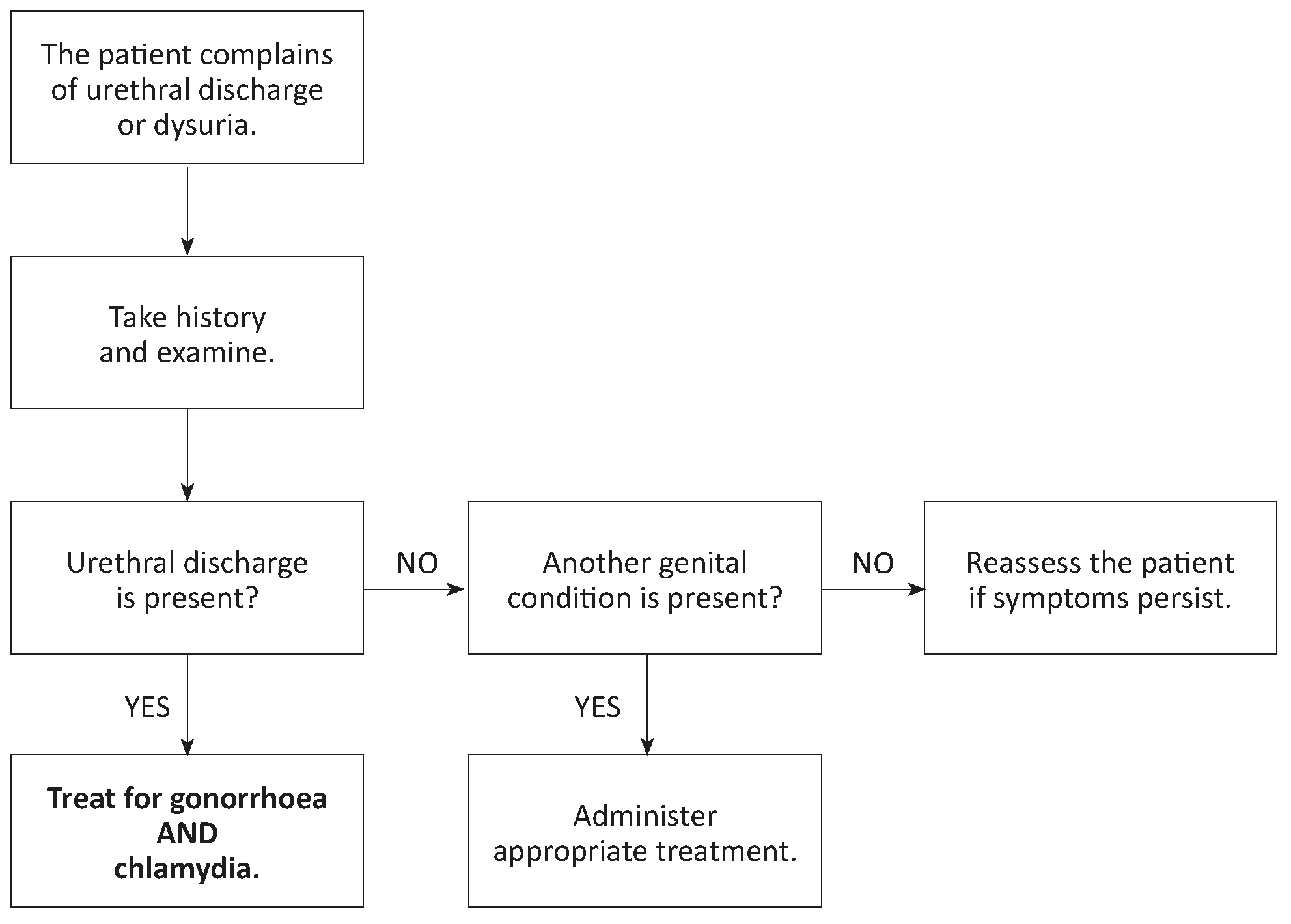
Abnormal discharge should be confirmed by performing a clinical examination aCitation a.In areas where lymphatic filariasis is endemic, be careful not to confuse purulent urethral discharge with milky or rice-water urine (chyluria) suggestive of lymphatic filariasis. . In males, the urethra should be milked gently if no discharge is visible. Furthermore, specifically check for urethral discharge in patients complaining of painful or difficult urination (dysuria).
Case management
Laboratory
- C. trachomatis cannot easily be identified in a field laboratory. In the absence of validated rapid diagnostic tests, the treatment is empiric.
- In men, a methylene blue or Gram stained smear from a urethral swab may be used to detect gonococci (Gram negative intracellular diplococci).
Treatment of the patient
- In women: same treatment as cervicitis.
- In men:
- If microscopy of a urethral smear has been performed: in the absence of gonococci, treat for chlamydia alone; in the presence of gonococci, treat for chlamydia AND gonorrhoea.
- When no laboratory is available, treat for chlamydia AND gonorrhoea as below:
If urethral discharge persists or reappears after 7 days:
- Verify that the patient has received an effective treatment (i.e. one of the combinations above).
- Gonococcal resistance is a possibility if another treatment (e.g. co-trimoxazole or kanamycin) has been administered: re-treat for gonorrhoea as above (chlamydia is rarely resistant).
- If an effective antibiotic therapy has been given, consider trichomoniasis (tinidazole or metronidazole PO, 2 g single dose); also consider reinfection.
Treatment of the partner
The sexual partner receives the same treatment as the patient, whether or not symptoms are present.
- (a)In areas where lymphatic filariasis is endemic, be careful not to confuse purulent urethral discharge with milky or rice-water urine (chyluria) suggestive of lymphatic filariasis.