On this page
Abnormal implantation of the placenta in the lower uterine segment, rather than in the uterine fundus.
The primary risk factors for placenta praevia are multiparity and a history of caesarean section.
Even under good circumstances (possibility of blood transfusion, high quality surgical setting), maternal and foetal mortality and the risk of postpartum haemorrhage are high.
3.1.1 Different types of placenta praevia
There are 4 types of placenta praevia:
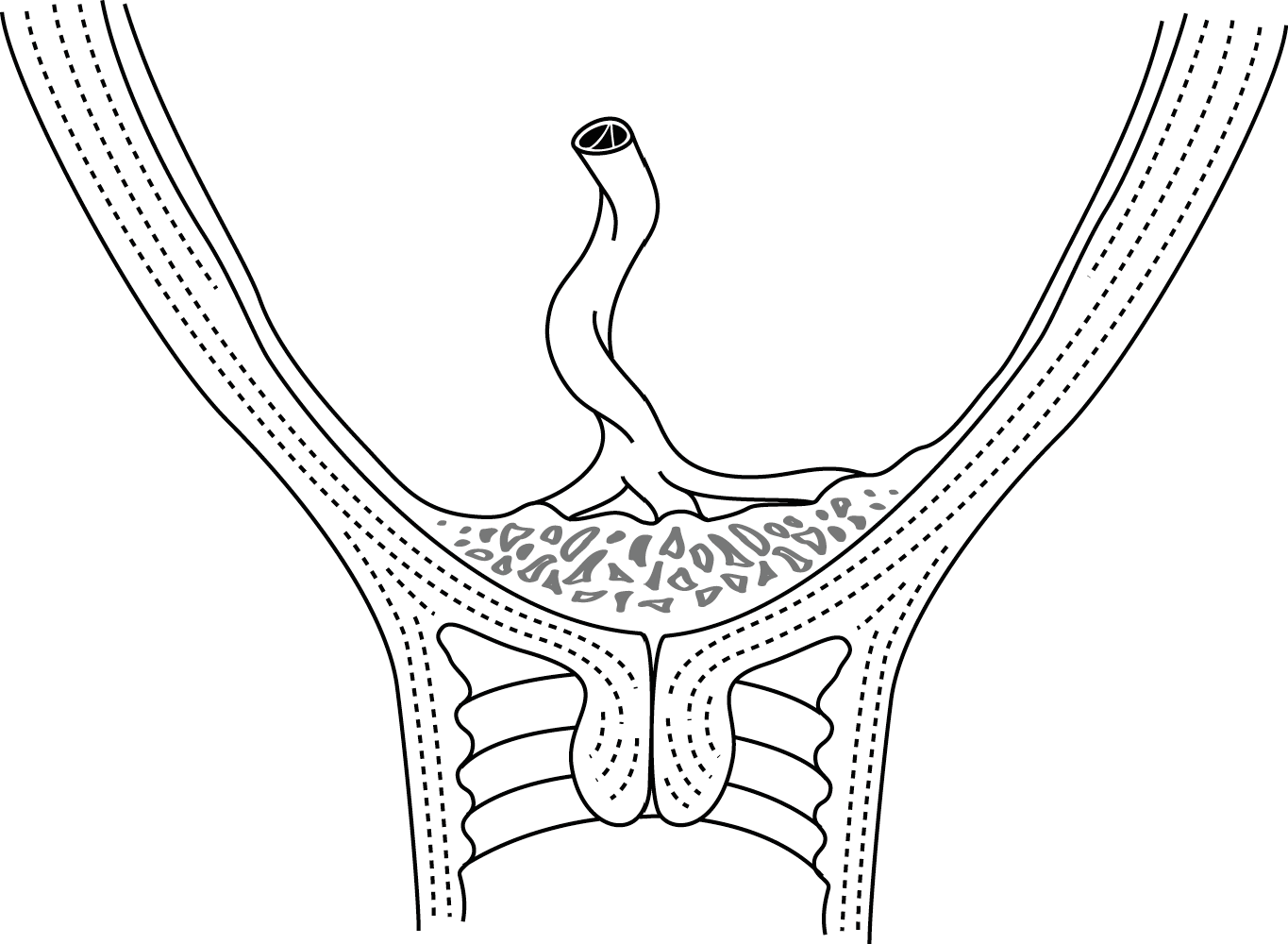
- Complete placenta praevia (Figure 3.1a), in which the placenta completely covers the internal cervical os;
- Partial placenta praevia, in which the placenta partially covers the internal cervical os;
In either of these cases, vaginal delivery is not possible. - Marginal placenta praevia (Figure 3.1b), in which the placenta touches, but does not overlap, the internal os;
- Lateral placenta praevia, in which the placenta is inserted in the lower segment, but more than 2 cm from the internal cervical os.
Figures 3.1 - Placenta praevia
 |
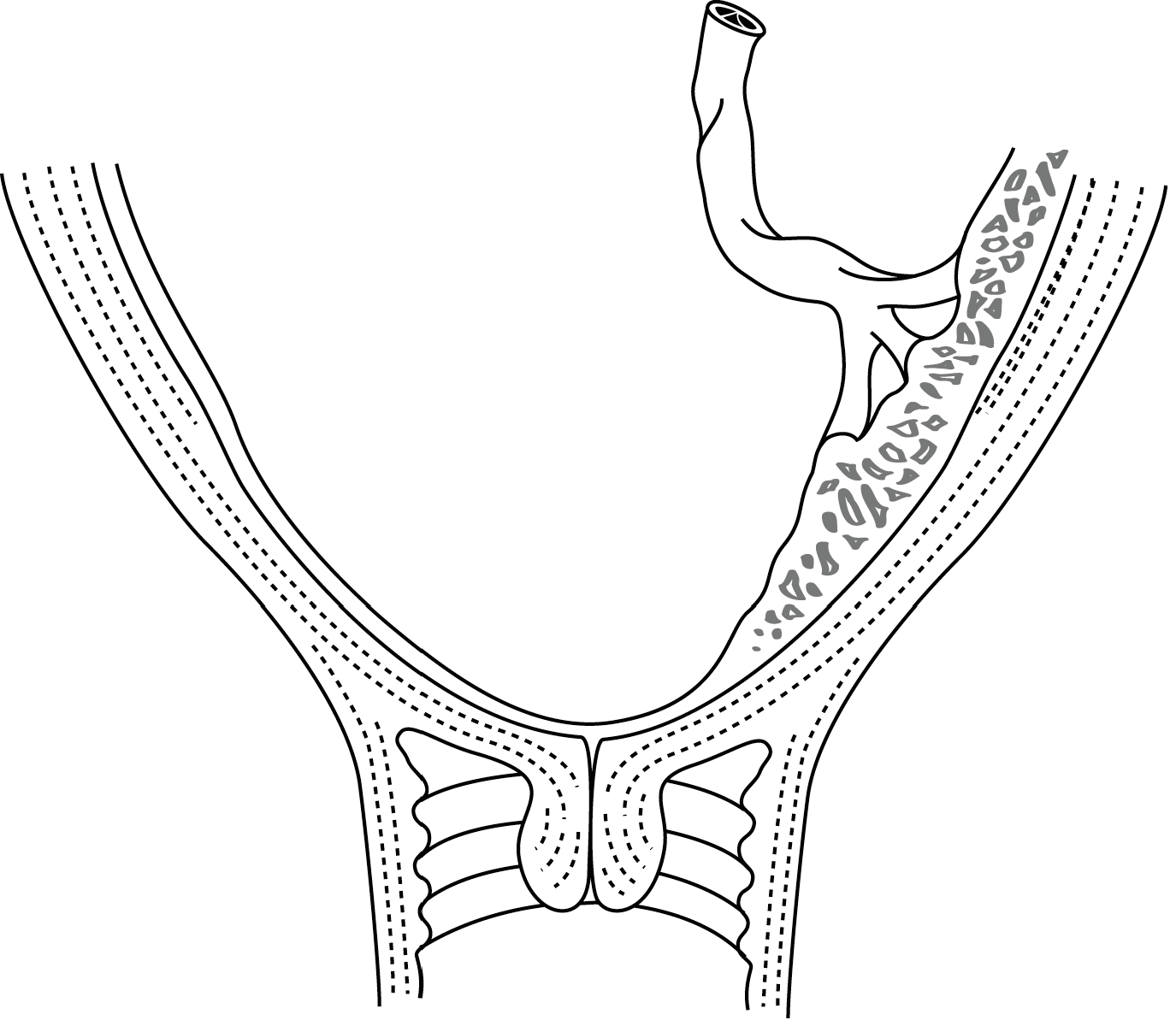 |
| 3.1a - Complete | 3.1b - Marginal |
3.1.2 Diagnosis
Signs and symptoms
In a woman more than 22 weeks LMP:
- Sudden, bright red bleeding associated with uterine contractions (not always felt by the patient).
- The foetus often presents high, pushed up by the placenta; the uterus is soft.
- Foetal heart tone usually heard.
- Examination with a speculum shows blood flowing from the cervical os.
Ultrasound
Ultrasound is the method of choice for diagnosing placenta praevia. It makes it possible:
- To avoid a vaginal examination that may trigger massive haemorrhage.
- To determine whether or not the placenta is covering the cervix, and thus the preferred route of delivery.
If ultrasound is not available or is not reliable, careful digital vaginal examination may be performed but only in the operating room, with resources at hand for immediate management of massive haemorrhage (IV line(s), transfusion, emergency caesarean section if necessary). Digital vaginal examination may reveal displacement of the cervix and deformation of the lower uterine segment by the placenta praevia. Rather than the hard foetal presentation, one feels a spongy mass. If possible, try to determine whether the placenta covers the entire cervix, or only part.
Once the diagnosis is established, do not perform another digital vaginal examination.
Once the diagnosis is established, do not perform another digital vaginal examination.
3.1.3 Management
- Insert an IV line (16-18G catheter) and administer Ringer lactate.
- Measure heart rate and blood pressure; assess the severity of the bleeding, measure haemoglobin.
- Prepare for a possible transfusion, determine the patient’s blood type, select potential donors or ensure that blood is available. If transfusion is necessary, only use blood that has been screened (HIV-1, HIV-2, hepatitis B, hepatitis C, syphilis, and malaria in endemic areas).
- If the uterus is scarred or there is a history of placenta praevia, consider the possibility of placenta accreta and prepare to perform a hysterectomy.
- If anaemia is present, treat according to severity.
Labour has not yet started and bleeding is minor to moderate
- Rest and monitoring: a sudden, massive haemorrhage is always possible, even if bleeding has completely stopped.
- In the event of complete or partial placenta praevia:
- the patient should remain hospitalized or close to a CEmONC facility;
- prolong the pregnancy, if possible, up to at least 34 weeks LMP (before 34 weeks LMP, consider foetal lung maturation with dexamethasone, Chapter 4, Section 4.10.2).
- Perform a caesarean section:
- between 34 and 37 weeks LMP, despite prematurity, if the situation is unstable (recurrent bleeding);
- after 37 weeks LMP after a single episode of bleeding that has stopped.
Labour has not yet started and bleeding is heavy
- Try a tocolytic agent to reduce contractions and bleeding (Chapter 4, Section 4.10.2).
- At the same time, prepare for caesarean section (regardless of the placenta's position or foetal viability), in case the bleeding persists or there is massive, uncontrolled bleeding (caesarean section to save the life of the mother).
- In remote areas, arrange a transfer to a CemONC facility. Be careful of the risk of exacerbating the bleeding if transport conditions are difficult.
Labour has started
- Complete placenta praevia and/or heavy bleeding: caesarean section.
- Placenta praevia not complete and minor bleeding: attempt vaginal delivery; rupture the membranes as soon as they are accessible, in such a way that the foetal head compresses the placental vessels and cuts off the bleeding.
Be careful of postpartum haemorrhage, which is common with all forms of low-lying placenta, due to the weaker retraction of the lower uterine segment. Do not hesitate to remove the placenta manually and explore the uterine cavity. Administer oxytocin routinely (Chapter 8, Section 8.1).