Nephrotic syndrome (NS) is characterized by the presence of oedema, heavy proteinuria, hypoalbuminemia, and hyperlipidaemia.
Primary or idiopathic NS is the most common cause of NS in children between 1 and 10 years. It usually responds to corticosteroids.
Secondary NS is associated with infectious diseases (e.g. post-infectious glomerulonephritis, endocarditis, hepatitis B and C, HIV infection, malaria, and schistosomiasis) and may respond to treatment of the underlying cause.
Children with NS are at increased risk of thromboembolism, severe bacterial infections (in particular, due to S. pneumoniae) and malnutrition. Untreated NS may progress to renal failure.
Clinical features
- Typically, the child presents with soft, pitting and painless oedema, which varies in location based on position and activity. Upon awaking, the child has periorbital or facial oedema, which over the day decreases as oedema of the legs increases.
As oedema worsens, it may localize to the back or genitals, or become generalized with ascites and pleural effusions.
- This oedema should be differentiated from the oedema of severe acute malnutrition (SAM): in SAM, the child presents with bilateral pitting oedema of the feet and lower legs that does not vary with position. Oedema extends upwards to hands and face in severe cases. It is usually associated with typical skin and hair changes (see Kwashiorkor: Severe acute malnutrition, Chapter 1).
- Once SAM is excluded, the following two criteria must be met to make a clinical diagnosis of primary NS:
- Presence of heavy proteinuria,
and - Absence of associated infections: see Hepatitis B and C and HIV infection (Chapter 8), Malaria and Schistosomiases (Chapter 6).
- Presence of heavy proteinuria,
Laboratory
- Urine
- Measure protein with urinary dipstick on three separate voided urine samples (first voided urine if possible). In NS, proteinuria is equal or greater than +++ or equal or greater than 300 mg/dl or 30 g/litreaCitation a.Nephrotic range proteinuria in children is defined as urinary protein excretion greater than 50 mg/kg daily. Quantitative measurement of protein excretion is normally based on a timed 24-hour urine collection. However, if this test cannot be performed, urine dipstick measurements can be substituted.. NS is excluded if heavy proteinuria is not consistently present.
- In case of macroscopic haematuria, or microscopic haematuria ≥ +, consider glomerulonephritis.
- Blood tests (if available)
- Serum albumin concentration less than 30 g/litre and hyperlipidaemia.
- Blood urea nitrogen (BUN) and creatinine most often in the normal range.
- Perform all necessary laboratory tests to exclude secondary NS.
Treatment
- Hospitalize the child for initial therapy.
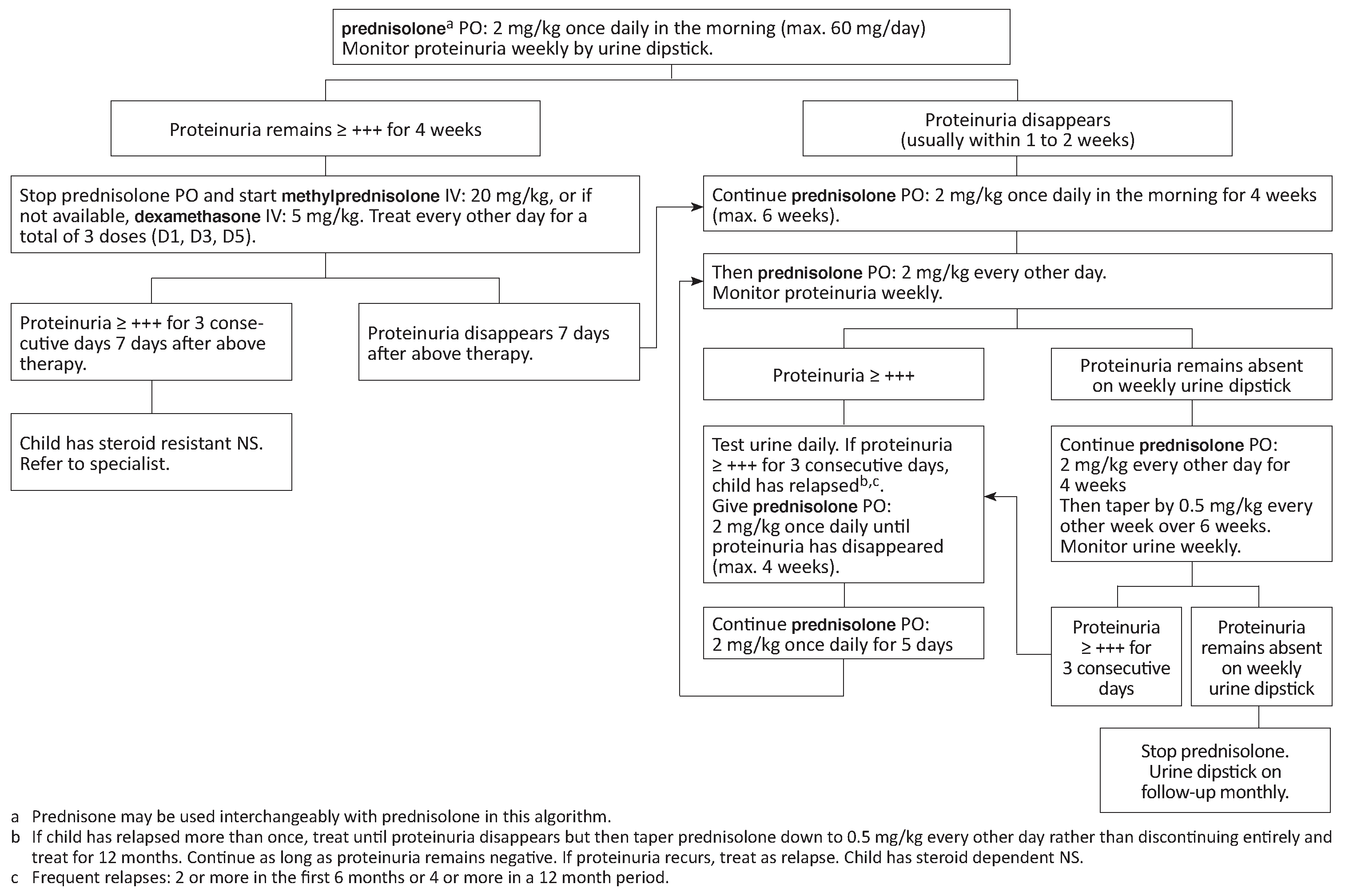
- Corticosteroids (prednisolone or prednisone) are indicated in primary NS.
- Before starting corticosteroid treatment:
- Treat any concomitant acute infections such as pneumonia, peritonitis, sepsis, pharyngitis, or cellulitis.
- Exclude active tuberculosis and/or start antituberculous treatment.
- Corticosteroid treatment
See algorithm below. Total length of initial treatment is 2 to 4 months.
- Nutrition, fluid intake, nursing and follow-up
- No salt-added diet.
- Do not restrict fluids (risk of thrombosis due to hypercoagulability). If oedema is very severe, fluids may initially be restricted (e.g. 75% of usual intake) while monitoring urine output.
- Encourage child to walk and play to prevent thromboembolism.
- Discharge child when stable, follow-up at least monthly, more frequently if indicated, weight and urine dipstick at each visit.
- Instruct the parent to continue no salt-added diet and to seek medical advice in case of fever, abdominal pain, respiratory distress or signs of thromboembolism.
- Management of infections
Treat infections as soon as they appear but do not routinely give prophylactic antibiotics.
- Immunization
- Children under 5 years: check that the child has received all EPI vaccines including Haemophilus influenzae type B, conjugated pneumococcal vaccine and (if in an endemic area) meningococcal A conjugate vaccine. If not, administer catch-up vaccines.
- Children over 5 years: check that the child has received tetanus, measles, pneumococcal conjugate and (if in an endemic area) meningococcal A conjugate vaccine. If not, administer catch-up vaccines.
Management of complications
- Intravascular volume depletion potentially leading to shock, present despite oedematous appearance
Signs include decreased urine output with any one of the following: capillary refill ≥ 3 seconds, poor skin perfusion/mottling, cold extremities, low blood pressure.
If signs are present, administer human albumin 5% IV: 1 g/kg. If albumin is not available, administer Ringer lactate or 0.9% sodium chloride: 10 ml/kg over 30 minutes.
If signs of shock are present, see Shock, Chapter 1.
- Respiratory distress due to severe oedema (rare)
This is the only situation in which diuretics should be used and only if there are no signs of intravascular volume depletion or after hypovolaemia has been corrected:
furosemide PO: 0.5 mg/kg 2 times daily
If not effective, discontinue furosemide. If creatinine is normal, administer spironolactone PO: 1 mg/kg 2 times daily. The dose can be increased to 9 mg/kg daily in resistant cases of ascites.
While on diuretics, monitor for dehydration, thromboembolism and hypokalaemia.
Specialized advice and management (including further investigations such as renal biopsy) are required:
- In children less than 1 year or more than 10 years,
- In case of steroid resistant NS,
- In case of mixed nephrotic and nephritic clinical picture.
In case of steroid-resistant NS, when referral is impossible and as a last resort, the following palliative measure may reduce proteinuria and delay renal failure:
enalapril PO: 0.1 to 0.3 mg/kg 2 times daily (start with the lowest dose and increase gradually if necessary until reduction of proteinuria). If available, monitor for hyperkalaemia.
This is a palliative measure and the prognosis for steroid-resistant NS is poor in the absence of specialized treatment.
- (a)Nephrotic range proteinuria in children is defined as urinary protein excretion greater than 50 mg/kg daily. Quantitative measurement of protein excretion is normally based on a timed 24-hour urine collection. However, if this test cannot be performed, urine dipstick measurements can be substituted.