Last updated: August 2022
Abnormal vaginal discharge is defined as discharge that is different from usual with respect to colour/odour/consistency (e.g. discoloured or purulent or malodorous).
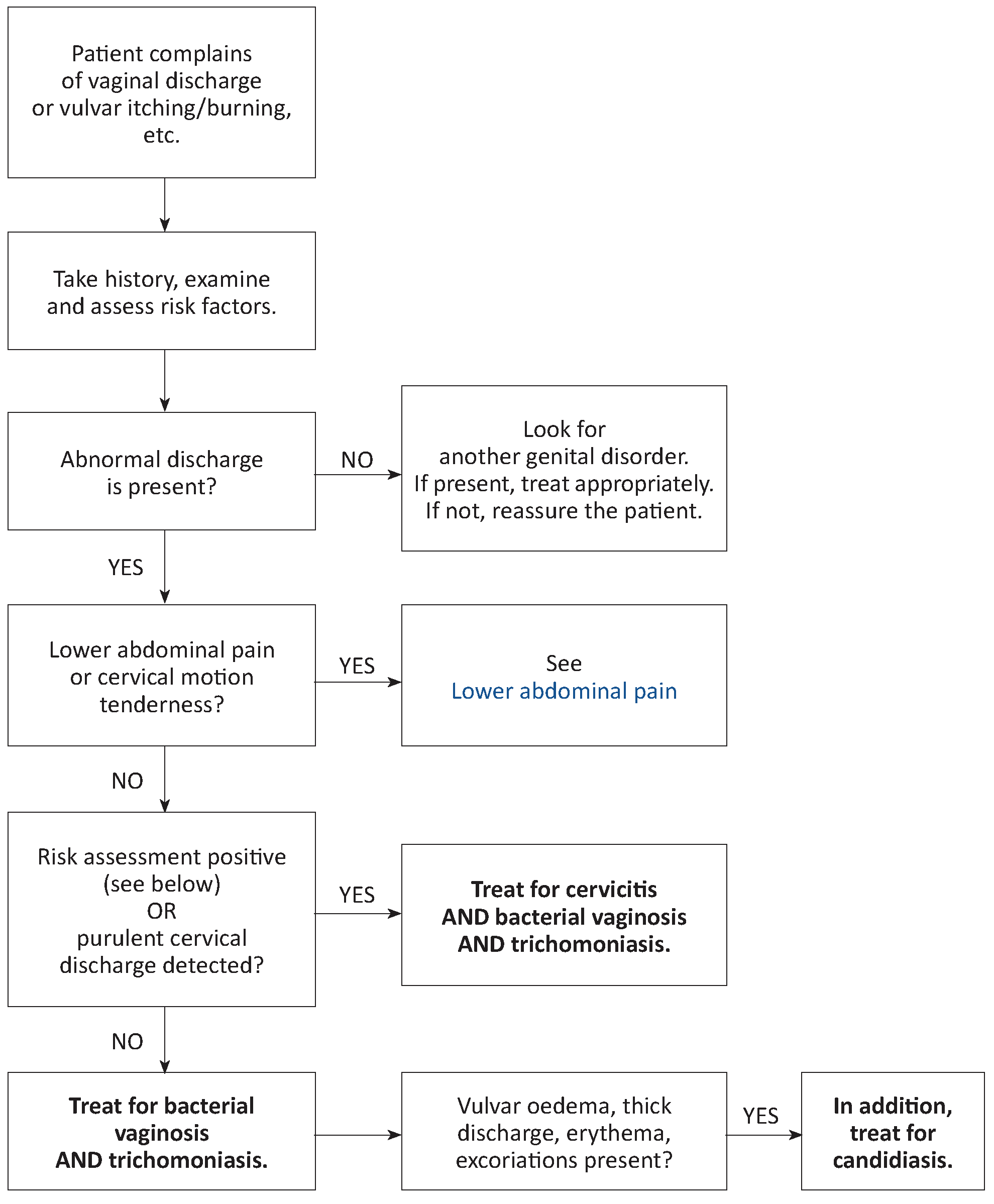
Abnormal discharge is often associated with vulvar pruritus or pain with intercourse (dyspareunia), or painful or difficult urination (dysuria) or lower abdominal pain. Routinely check for abnormal vaginal discharge in women presenting with these symptoms.
Abnormal vaginal discharge may be a sign of infection of the vagina (vaginitis) and/or the cervix (cervicitis) or upper genital tract infection.
Abnormal discharge must be clinically confirmed: inspection of the vulva, speculum exam checking for cervical/vaginal inflammation or discharge.
Abdominal and bimanual pelvic examinations should be performed routinely in all women presenting with vaginal discharge to rule out upper genital tract infection (lower abdominal pain and cervical motion tenderness).
The principal causative organisms are:
- In vaginitis: Gardnerella vaginalis and other bacteria (bacterial vaginosis), Trichomonas vaginalis (trichomoniasis) and Candida albicans (candidiasis).
- In cervicitis: Neisseria gonorrhoeae (gonorrhoea) and Chlamydia trachomatis (chlamydia).
- In upper genital tract infections: see Upper genital tract infections.
Case management
Cervicitis may be difficult to diagnose. When in doubt, administer treatment for cervicitis to women with abnormal vaginal discharge and any of the following risk factors:
- Urethral discharge in the partner
- Context of sexual violence or prostitution
- New partner or more than one partner in the preceding 3 months
Laboratory
- Xpert molecular (PCR) tests are recommended for the detection of C. trachomatis and N. gonorrhoea.
- Microscopic examination of a fresh wet smear may show mobile T. vaginalis, yeast cells and hyphae in candidiasis, and “clue cells” in bacterial vaginosis.
- Identification of N. gonorrhoeae by Gram-stained smear is not sensitive in women and is not recommended.
Treatment of the patient
Cervicitis
Treat for both chlamydia AND gonorrhoea.
| Treatment for chlamydia | Treatment for gonorrhoea | |
|---|---|---|
| Non-pregnant women | ||
|
azithromycin PO: 1 g single dose |
PLUS |
ceftriaxone IM: 500 mg single dose |
| Pregnant women | ||
| azithromycin PO: 1 g single dose or erythromycin PO: 1 g 2 times daily or 500 mg 4 times daily for 7 days |
PLUS | ceftriaxone IM: 500 mg single dose or, if not available, cefixime PO: 400 mg single dose |
Bacterial vaginosis and trichomoniasis
tinidazole PO: 2 g single dose
or metronidazole PO: 2 g single dose
In the case of treatment failure:
tinidazole PO: 500 mg 2 times daily for 5 days
or metronidazole PO: 400 to 500 mg 2 times daily for 7 days
Vulvovaginal candidiasis
clotrimazole (500 mg vaginal tab): 1 tablet inserted deep into the vagina at bedtime, single dose
If the patient has extensive vulvar involvement, miconazole 2% cream (one application to the vulva 2 times daily for 7 days) may be used in combination with the intravaginal treatment above. Miconazole cream may complement, but does not replace, treatment with clotrimazole.
Treatment of the partner
When the patient is treated for vaginitis or cervicitis, the partner receives the same treatment as the patient, whether or not symptoms are present.
In the case of vulvovaginal candidiasis, the partner is treated only if symptomatic (itching and redness of the glans/prepuce): miconazole 2% cream, one application 2 times daily for 7 days.