A transverse lie constitutes an absolute foeto-pelvic disproportion, and vaginal delivery is impossible.
This is an obstetric emergency, because labour is obstructed and there is a risk of uterine rupture and foetal distress.
7.6.1 Diagnosis
- The uterus is very wide: the transverse axis is virtually equivalent to the longitudinal axis; fundal height is less than 30 cm near term.
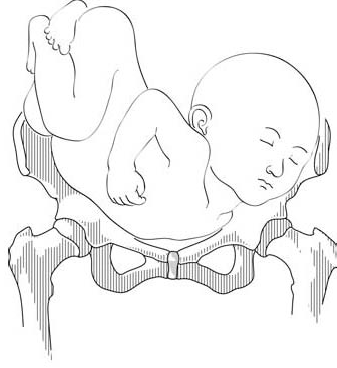
- On examination: head in one side, breech in the other (Figures 7.1a and 7.1b). Vaginal examination reveals a nearly empty true pelvis or a shoulder with—sometimes—an arm prolapsing from the vagina (Figure 7.1c).
Figures 7.1 - Transverse lie and shoulder presentation
|
|
7.1b - Dorso-superior (back up) left shoulder presentation |
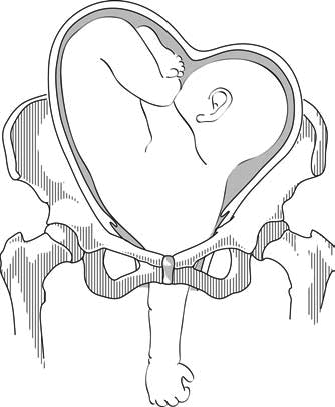
7.1c - Neglected shoulder presentation
7.6.2 Possible causes
- Grand multiparity (5 deliveries or more)
- Uterine malformation
- Twin pregnancy
- Prematurity
- Placenta praevia
- Foeto-pelvic disproportion
7.6.3 Management
This diagnosis should be made before labour begins, at the last prenatal visit before the birth.
At the end of pregnancy
Singleton pregnancy
- External version 4 to 6 weeks before delivery, in a CEmONC facility (Section 7.7).
- If this fails, delivery should be carried out by caesarean section, either planned or at the beginning of labour (Chapter 6, Section 6.4.1).
Twin pregnancy
- External version is contra-indicated.
- If the first twin is in a transverse lie (unusual): schedule a caesarean section.
- If the second twin is in a transverse lie: there is no indication for caesarean section, but plan delivery in a CEmONC facility so that it can be performed if necessary. Deliver the first twin and then, assess the foetal position and give a few minutes for the second twin to adopt a longitudinal lie. If the second twin stays in a transverse lie, and depending on the experience of the operator, perform external version (Section 7.7) and/or internal version (Section 7.8) on the second twin.
During labour, in a CEmONC facility
Foetus alive and membranes intact
- Gentle external version, between two contractions, as early as possible, then proceed as with normal delivery.
- If this fails: caesarean section.
Foetus alive and membranes ruptured
- Complete dilation:
- Multipara with relaxed uterus and mobile foetus, and an experienced operator: internal version and total breech extraction.
- Primipara, or tight uterus, or immobile foetus, or engaged arm, or scarred uterus or insufficiently-experienced operator: caesarean section.
- Incomplete dilation: caesarean section.
Caesarean section can be difficult due to uterine retraction. Vertical hysterotomy is preferable. To perform extraction, grasp a foot in the fundus (equivalent to a total breech extraction, but by caesarean section).
Foetus dead
Embryotomy for transverse lie (Chapter 9, Section 9.7.7).
During labour, in remote settings where surgery is not available
Foetus alive and membranes intact
Try to refer the patient to a CEmONC facility. If not feasible:
- Attempt external version as early as possible.
- If this fails, wait for complete dilation.
- Perform an external version (Section 7.7) combined with an internal version (Section 7.8), possibly placing the woman in various positions (Trendelenburg or knee-chest).
Foetus alive and membranes ruptured
Try to refer the patient to a CEmONC facility. If not feasible:
- Complete dilation:
- Put the woman into the knee-chest position.
- Between contractions, push the foetus back and try to engage his head.
- Vacuum extraction (Chapter 5, Section 5.6.1) and symphysiotomy (Chapter 5, Section 5.7) at the slightest difficulty.
- Incomplete dilation: Trendelenburg position and watchful waiting until complete dilation.
Foetus dead
Try to refer the patient, even if referral takes some time.
If not feasible, embryotomy for transverse lie (Chapter 9, Section 9.7.7).