Premature separation of the normally implanted placenta, prior to foetal expulsion with formation of a haematoma between the placenta and the uterine wall. The haematoma completely or partially separates the placenta from the uterine wall.
Abruptio placentae (or placental abruption) often occurs with trauma or in cases of hypertension or pre-eclampsia.
This can trigger a clotting disorder in the mother, with a risk of severe secondary haemorrhage (disseminated intravascular coagulation).
Emergency uterine evacuation (vaginal or caesarean) is needed to save the lives of the mother and foetus, no matter what the stage of pregnancy.
3.2.1 Diagnosis
Abruptio placentae is diagnosed clinically. It should be suspected when one or more of the following signs are present:
- Sudden, severe, continuous abdominal pain;
- Uterus in spasm, feels hard, “woody”;
- Sudden, light, blackish bleeding; the bleeding may be heavy if there is an associated clotting disorder;
- Shock, out of proportion to the severity of the external bleeding (intra-uterine bleeding): rapid or weak or undetectable pulse, very low or undetectable blood pressure; tachypnoea, pallor, sensation of cold, damp skin, agitation and anxiety.
- Foetal hypoxia, depending on the size of the placental abruption: foetal heart rate slows or foetal heart tone disappear.
- When the membranes rupture, the fluid is uniformly red.
Sometimes the picture is incomplete: there may be no vaginal bleeding or uterine spasm, or no foetal distress.
Ultrasound, when available, is useful for verifying foetal vitality.
3.2.2 Management
- Insert an IV line (16-18G catheter) and administer Ringer lactate.
- Measure heart rate and blood pressure; assess the severity of the bleeding. If there are no clots, consider the possibility of a clotting disorder.
- In remote areas, arrange a transfer to a CEmONC facility, if possible, in anticipation of the need to transfuse, perform a caesarean section or hysterectomy, and manage post-partum haemorrhage.
To assess clotting disorders
[1]Citation 1.World Health Organization. Managing complications in pregnancy and childbirth. A guide for midwives and doctors. Geneva 2017.
http://apps.who.int/iris/bitstream/handle/10665/255760/9789241565493-eng.pdf?sequence=1
:
- Take 2 ml of blood into a dry, clean, glass tube (approximately 10 mm x 75 mm).
- Hold the tube in a closed fist to keep it warm (± 37 °C).
- After 4 minutes, tip the tube slowly to see if a clot is forming then, tip it again every minute until the blood clots and the tube can be turned upside down.
- Failure of a clot to form after 7 minutes or a soft clot that breaks down easily suggests clotting disorders.
For blood transfusion:
- Determine the patient’s blood type;
- Select potential donors for possible transfusion of fresh whole blood;
- If transferred, the woman should be accompanied by family members who are potential blood donors;
- If there is moderate bleeding and no clotting disorder, transfuse packed red blood cells or whole blood;
- If there is massive bleeding and/or a clotting disorder, transfuse fresh whole blood (drawn less than 4 hours and unrefrigerated) or packed red blood cells or whole blood combined with fresh frozen plasma;
- Blood or other blood products must have been screened (HIV-1, HIV-2, hepatitis B, hepatitis C, syphilis, and malaria in endemic areas).
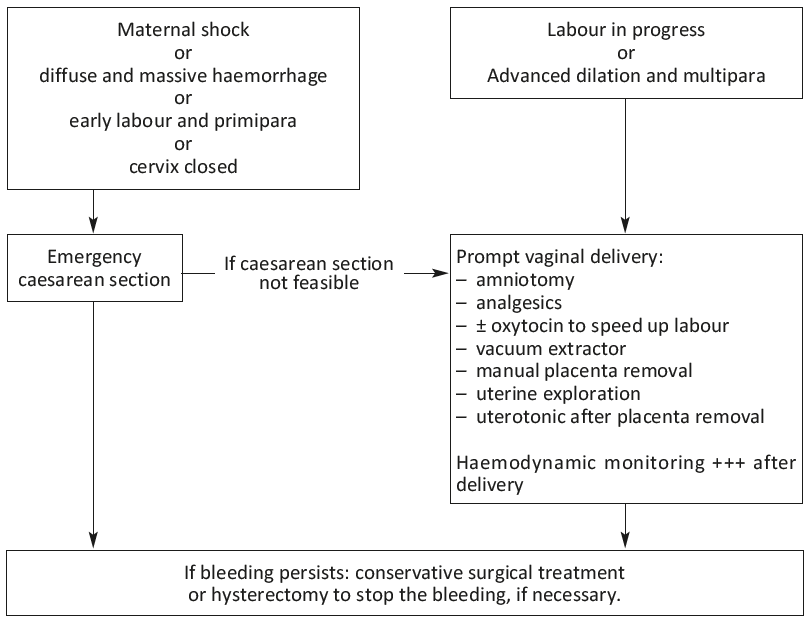
Delivery should be done quickly, ideally before the onset of clotting disorders. When not indicated initially, caesarean section becomes imperative if labour progresses too slowly – even in the event of intrauterine foetal death.
Management of abruptio placentae
- 1.World Health Organization. Managing complications in pregnancy and childbirth. A guide for midwives and doctors. Geneva 2017.
http://apps.who.int/iris/bitstream/handle/10665/255760/9789241565493-eng.pdf?sequence=1