The aim of the investigation is to collect the data needed to confirm the outbreak and analyse the initial actions taken in response.
The effectiveness of the response (controlling the spread of the outbreak by organising a large-scale vaccination campaign) depends primarily on how quickly the outbreak is identified.
The investigation must therefore start at the first warning signs, i.e., an increase in the number of cases compared to the same period in previous (non-epidemic) years.
In principle, if the epidemiological surveillance system is functional and responsive, the alert will be issued as soon as the first cases appear.
3.2.1 Defining cases
The description of an outbreak rests on the case definition. The case definition should be clear, simple and standardised, so that it can be used at all levels from health post to hospital. It should remain constant for the duration of the outbreak. Standardisation allows uniform data collection, i.e., the number of cases and deaths, the age groups at risk and the geographic extent.
The following (WHO-recommended) case definitions are given as an illustration:
| Suspected case |
Any person in whom a clinician suspects measles infection |
|---|---|
| Probable case |
Suspected case |
| Confirmed case |
Suspected or probable case
|
All case definitions are a compromise. A sensitive but relatively nonspecific definition will include all of the cases, but will also include patients who are not cases (overestimation).
Conversely, if the definition is highly specific, all cases counted will be true cases, but some true cases will not be included (under estimation).
3.2.2 Confirming the diagnosis
Most of the time, the diagnosis is clinical (based on the definition of a suspect case).
Prior to the eruptive (rash) phase, suspicion of the disease is based only on contact with a patient and no past history of measles. After the eruptive phase, it requires a differential diagnosis from other febrile eruptive illnesses and drug reactions (Chapter 5).
Laboratory confirmation
Laboratory testing is crucial to confirm an outbreak, but inability to get laboratory confirmation must not delay outbreak management.
Specimen collection equipment should be made available at all levels (hospitals, health facilities, etc.) at the start of the high-risk season, so that samples can be taken at the first contact with the patient.
At a minimum, specimens should be collected on the first five to ten reported cases in an affected geographic area.
Serological testing for IgM antibody is most sensitive if done between the 3rd and 28th day after onset of the skin eruption. It should therefore be done during that period, if possible. After labelling the tube and completing the sample register (Appendix 2), quickly send the tube to the laboratory, accompanied by a completed information form (Appendix 3).
Follow the specimen collection procedures recommended by the country’s Ministry of Health.
There are three possible methods for collecting specimens
[1]Citation 1.World Health Organization. Manual for the laboratory diagnosis of measles and rubella infection, 2nd ed. CH-1211 Geneva 27, Switzerland (WHO/IVB/07.01).
http://apps.who.int/iris/bitstream/handle/10665/70211/WHO_IVB_07.01_eng.pdf?sequence=1&isAllowed=y
(Appendix 4):
- collecting capillary blood, dried, on filter paper;
- swabbing the oral mucosa (between the gum and the tooth) using a small sponge;
- collecting whole blood or serum by venipuncture.
For simplicity and safety, dried blood samples or oral fluid swabs are preferred to serum, because:
- they have nearly equivalent sensitivity and specificity for detection of specific IgM antibodies;
- they do not require venipuncture;
- they permit IgM detection and strain identification;
- the samples are stable for about 7 days without a cold chain.
The result is:
- positive if there is > 20% difference between the levels of measles-specific IgM antibodies and the control;
- negative if the difference is < 10%;
- invalid (equivocal) if the difference is between 10 and 20%.
| During an outbreak, laboratory confirmation testing is done on the first several cases (in each geographic area). Once measles is confirmed, epidemiological surveillance relies on the clinical definition (suspected cases). |
3.2.3 Counting cases and deaths
The methods for finding cases will depend on the population in question and the existing surveillance system. Cases are looked for and counted:
- at hospitals, health facilities, dispensaries and feeding centres (counting the cases in the registers) first;
- in schools and other places where there are groups of children;
- more rarely, in the villages, by questioning the village heads and visiting the families of reported cases, or cemeteries.
If health care facilities do not have measles registers, put them in place (Appendix 5).
For each reported case, collect the following information: name, date of birth (or age, if date of birth unavailable), sex, address, admission date, treatment, outcome (recovery, death, or transfer), vaccination status and, if possible, vaccination date.
To avoid double reporting, it is essential to specify how transferred cases are counted.
Cases are reported from the beginning to the end of the outbreak.
3.2.4 Demographic data
The demographic data provide the denominator needed for calculating several indicators (incidence and attack rate).
Reliable demographic data can be hard to get. Often, there are no public records. Be aware of over- and underestimations, depending on the source.
It is important to get the most accurate possible data. Compare the data from several different sources. Justify the choice of data used, and give the source. There should be consensus among the main partners.
For example, demographic data from an old census can be used by applying the hypothetical annual population growth rate.
Local authorities may have more recent population figures than those available at the national level.
Everyone involved in managing the outbreak must use the agreed-upon population data until the en of the outbreak.
3.2.5 Organizing the data
This is the descriptive stage of the outbreak investigation. The situation is described in terms of time, place, and person.
Time
The data are transferred chronologically from the data collection tables (Appendix 6) onto a graph. The epidemic curve obtained represents the distribution of cases by date of diagnosis (Figure 3.1).
This curve allows confirmation that there is an outbreak. If it is completed on regular basis, it also helps monitor the time course of the outbreak and assess the efficacy of the response.
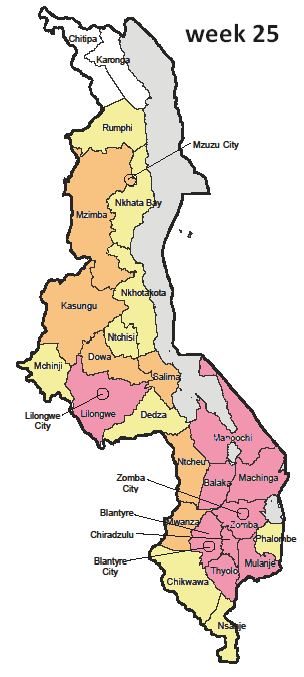
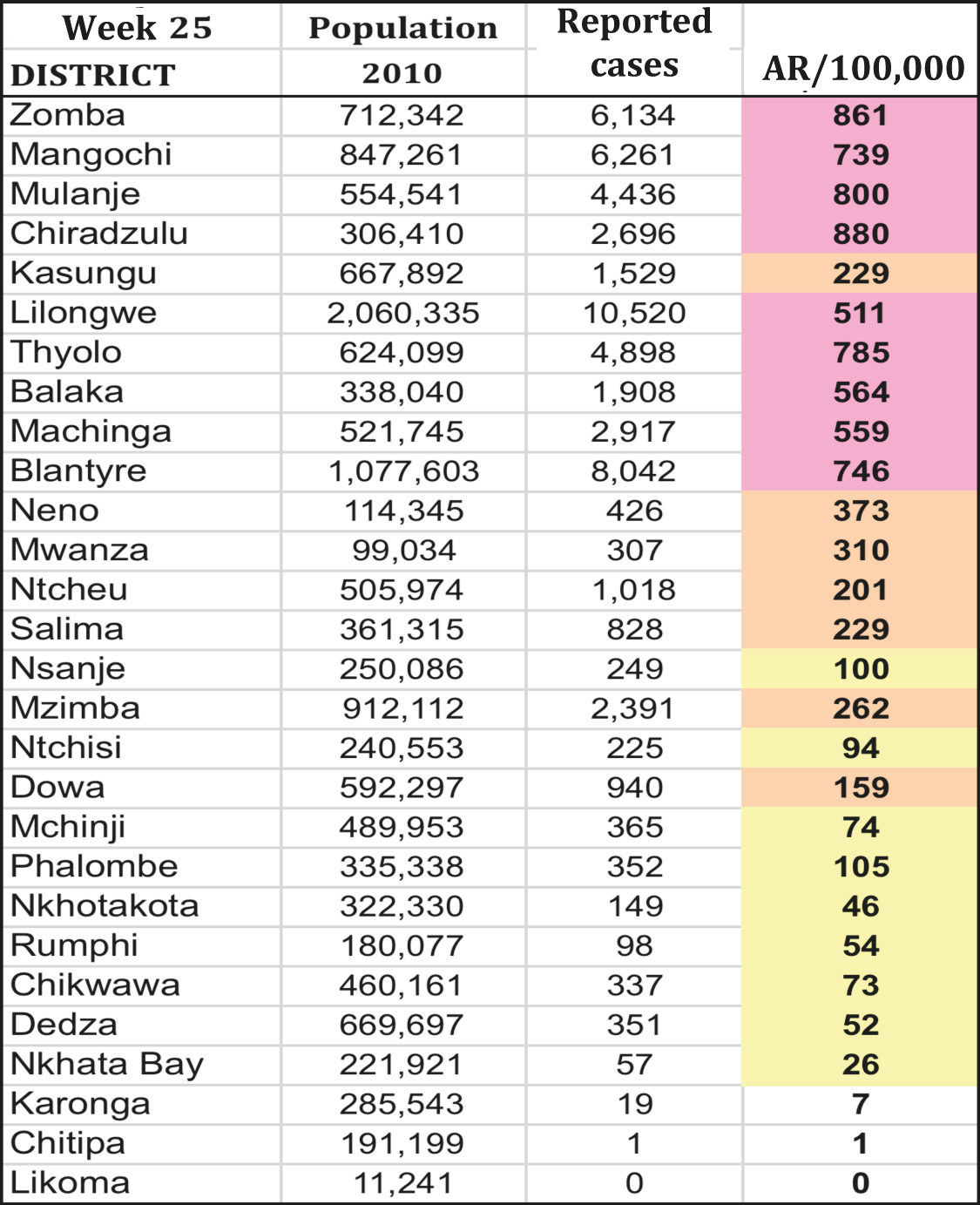
Figure 3.1: Reported measles cases by week, Malawi, 2010
Source: MoH/Epicentre
Place
The geographic distribution of cases or specific attack rates by geographic area (district/ neighbourhood/town or refugee camp section) helps visualise the extent of the outbreak and identify the highest risk areas, in order to set priorities in terms of response.
Figure 3.2: Geographic distribution of measles cases, Week 25, Malawi, 2010
 |
 |
Source: MoH/Epicentre
Person
While it is essential to determine the age of the cases, gender may also be a consideration.
The hardest-hit age groups are identified by calculating the age-specific attack rate. This indicator is critical in defining the target population for the vaccination campaign.
The suggested age groups to look at are 0-5 months, 6-8 months, 9-11 months, 12-59 months, 5-14 years and ≥ 15 years. Depending on the context, it may be necessary to divide the data into other age groups, e.g., 5-9 years and 10-14 years for children and 15-29 and ≥ 30 years for adults (Figure 3.3).
If the available demographic data do not include the distribution by age group, it is often possible to calculate it from the total population and national data used by other programmes (e.g., EPI). Failing that, use the standard population distribution (Appendix 7).
Figure 3.3: Measles attack rate by age group, Malawi, 2010
Source: MoH/Epicentre
3.2.6 Analysing the data
Analyse these data to:
- determine the speed with which the outbreak is spreading, and its size (epidemic curve);
- identify the at-risk populations (age groups and place);
- plan and adjust the response, in order to limit the number of deaths and cases and the spread of the outbreak (estimate the needs in terms of treatments, vaccine doses, etc.).
The main indicators to calculate for each level (region, district, town, etc.) are:
- the weekly and cumulative incidence (attack rate);
- the specific attack rate:
- by location (neighbourhood, health zone, commune, refugee camp zone),
- by age group (e.g., for a few health facilities).
- the weekly and cumulative case fatality rate:
- by age group,
- by treatment site (e.g., in-hospital mortality).
Weekly incidence
This is the speed with which a disease appears in the population during a given period. It is calculated each week during an outbreak.
Number of new cases during the week in question x 100,000
––––––––––––––––––––––––––––––––––––––––––––––––––––––––––
Total population
Example: in Week 3, there were 85 measles cases reported out of a population of 542,080. The incidence was: 85/542,080 x 100,000 = 15.7/100,000.
Attack rate
The attack rate is a particular form of the incidence. It is a cumulative incidence, calculated over a short period of time – since the start of the outbreak, in particular.
Number of new cases during a given period x 100
––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––
Population exposed to the risk of the disease during the same period
Example: there were 3,022 cases of measles reported in children under age 1 year during the four months of the outbreak. There were 20,057 children in that age group (3.7% of the population).
The measles attack rate in children < 1 year was: 3,022/20,057 x 100 = 15.1%.
Case fatality rate
The case fatality rate (CFR) is the percentage of deaths among cases of a disease. It is an indicator of the severity of the disease and the quality of patient management.
Number of deaths due to measles in a given place during a given period x 100
–––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––
Number of measles cases reported in the same place during the same period
Example: Of the 3,022 cases of measles reported in children under age 1 year, 250 died. 472 of them were treated at the hospital, where 118 of them died:
- The CFR for children under 1 year was: 250/3,022 x 100 = 8.3%
- The in-hospital mortality for children under 1 year was: 118/472 x 100 = 25%
- 1.World Health Organization. Manual for the laboratory diagnosis of measles and rubella infection, 2nd ed. CH-1211 Geneva 27, Switzerland (WHO/IVB/07.01).
http://apps.who.int/iris/bitstream/handle/10665/70211/WHO_IVB_07.01_eng.pdf?sequence=1&isAllowed=y