A CTC is an autonomous inpatient facility which has its own general services (latrines, showers, kitchen, laundry, morgue and waste area), stocks and resources (medical and logistics, water and electricity). It operates 24 hours a day.
6.1.1 Choice of site and premises
CTCs should preferably be set up within the grounds of existing health facilities (if the configuration of the site allows for patient isolation) or on an adjacent site. These sites are preferred as patients are familiar with them. They may also already have certain installations (e.g. water, showers, and latrines) which can be used for the CTC, which saves time.
If it is not possible to set up a CTC in or beside a health facility, a community building (hangar, sports hall, etc.) can be transformed into a CTC or a new facility can be built.
A CTC site must imperatively:
- Be centrally located, in order to allow access to the largest possible number of patients.
- Be accessible by road at all times (ambulances and deliveries).
If the Ministry of Health imposes a site, ensure these conditions are met.
Furthermore:
- The ground must be able to absorb waste water and allow the digging of latrines.
- The site must not be prone to flooding (must not lie in a basin); a slight incline facilitates the drainage of rainwater.
- There must be a distance of at least 1.5 metre between the water table and the bottom of the latrines, waste pit, excreta pit, etc.
- The site must be less than 30 metres from a water point (spring, well, borehole, river, lake) and at least 100 metres away from public places (market, housing).
Available sites may be limited. If one or more of the above conditions are not met, the specific constraints and risks involved must be carefully analysed, as well as the problems to be resolved.
If a CTC is to be built:
- In emergency situations, tents are usually used as they are quick to set up and allow the facility to be modified according to needs.
- Installing semi-permanent buildings takes longer (local purchasing of materials, recruitment of qualified workers, construction time) but has the advantage of lasting several years. These are better designed for endemic zones where treatment facilities are regularly re-opened during outbreak periods.
If transforming existing facilities into a CTC:
- Hangars and sports halls are large open spaces which can be transformed into a CTC.
- Schools are sometimes used. Often the building is divided into classrooms which will influence the layout of the CTC. Using a school as a CTC implies that teaching will be suspended during the outbreak; this should therefore only be envisaged as a last resort. Strictly avoid rooms that are too small (3 or 4 beds) where staff cannot be permanently present to observe patients as they are responsible for several rooms.
- In all events:
- Obtain authorisation to use the site (land, stadium, building, public or private property) and draw up a written contract that complies with local legal requirements.
- Existing requisitioned installations (latrines, showers, and kitchen) must be reserved for exclusive use by the CTC.
- Check water supply possibilities (source that is nearby with reliable, sufficient flow).
- The population may reject the installation of a cholera facility for fear of the disease, particularly if there has never be a cholera outbreak in the area. Ask the health promotion team to help deal with this type of problem.
6.1.2 Area required
Total surface area
The total surface area required is calculated on the basis of approximately 30 m² per patient. This area takes into account all the required services (hospitalisation, technical services, etc.). Nevertheless a larger surface area than required should be considered in order to expand the CTC if necessary.
For example: for a CTC of 100 beds about 3000 m² are immediately required, but if the site is 3800 m² at least 25 more beds can be added if needed.
Surface area per patient
A bedridden patient requires about 4 m² and a seated patient about 2 m². For example: in a 75 m² room, 17 beds (maximum 18) + one nurse station can be set up.
If tents are being used, a 45 m² tent can hold 10 beds + one nurse station. 45 m² tents can be put up in pairs if necessary.
The space available or allocated by authorities may not be big enough to build a CTC with the required number of beds. In this event set up several CTUs at strategic points.
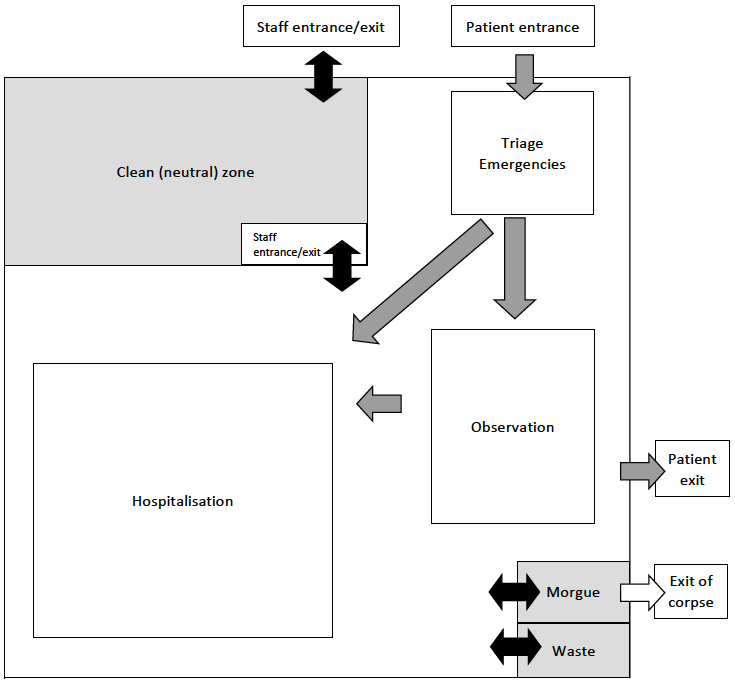
6.1.3 Layout and plan
Isolation
In a CTC patients are isolated from other hospitalised patients (if the CTC is within hospital grounds) and from the population. The CTC is separated from the exterior by a fence.
Separation of “contaminated” and “clean” zones
The CTC is composed of two distinct, separate areas:
| CONTAMINATED ZONE | CLEAN (or “neutral”) ZONE |
|
• Triage/Emergency |
• Stock/Administration |
The “contaminated” zone is where the vibrio is usually present in large quantities because of the presence of patients, corpses (morgue) and objects contaminated by patients (laundry, surfaces, dishes and waste).
The “clean” or “neutral” zone is reserved for administration, staff (offices, changing rooms, etc.) and stock (medical, logistics, food, water storage). Meals are prepared in this area. Chlorine solutions are also prepared in this area. Patients and attendants are not allowed to enter the clean zone.
Clearly separate the two zones with an interior barrier. Leave a passage between the two zones through which staff can enter and circulate in the contaminated area to treat patients and supply the wards with drugs, water, chlorine solutions, meals, etc.
See Appendix 11 for an example of a CTC layout.
6.1.4 Circulation of patients, attendants and staff
See also Chapter 7.
Set up entry/exit points to the exterior
The CTC compound has 4 points of entry/exit:
For patients
- A guarded door reserved for the entry of patients. All patients enter through this door and are directed to triage.
- A guarded door reserved for the exit of patients. All patients who have completed treatment (cured) or who are not admitted (e.g. illness other than cholera), leave by this door.
Depending on the context, it is not always possible to have a separate entrance and exit but this remains the best option, especially in large CTCs.
For staff and suppliers
A guarded gate, opening into the clean zone, reserved for the entry and exit of staff and supply vehicles.
For deceased patients
A locked door (not guarded) to the morgue for the collection of corpses.
Delimit sectors within the contaminated zone
- Delimit each healthcare sector (triage, observation, hospitalisation, etc.). Patients and attendants must not be allowed to circulate freely on their own initiative.
- Delimit sectors forbidden to patients: morgue and waste area.
Circulation of patients, attendants and staff in the CTC
6.1.5 Equipment
Cholera kits
Cholera kits are designed to facilitate operations, especially at the beginning of an outbreak. They contain medical and logistic materials to set up a CTC aCitation a.For the MSF kit, see the MSF kit catalogue. .
Other equipment
Not everything needed to set up a CTC is contained in the kits (or there is not a sufficient amount of certain articles). Supplementary materials need to be ordered at the same time as the kit or bought, or made, on-site (e.g. tents, plastic sheeting, cholera beds or chairs, staff clothing, etc.).
6.1.6 Signage
Put up clear signage for patients (signs, posters, symbols, pictures, text in the local language):
- Near the entrance to the CTC
If the CTC is within hospital grounds, put up signs giving directions to the CTC so as to avoid cholera patients entering other services.
- At the entrance of the CTC
- Put up a Patient Entrance sign.
- Put up a Staff and Suppliers Entrance sign.
- Inside the CTC
- Put up a No Entry sign (staff only) at the entrance to the clean zone, morgue and waste area.
- Label containers: ORS, potable water, 0.05% chlorine solution for hand-washing.
- Put up a sign indicating men’s/women’s showers and the latrines.
- Put up a No Entry sign to excreta pits (they must not be used by patients).
6.1.7 Setting up a CTC
The example below is of a CTC built from scratch using tents, in order to describe all the installations required. If a CTC is installed in a ready-built, partially equipped site then adaptions are needed, but the layout principles and order of priorities remain the same.
In the first 24 hours
The priority actions are presented in a list below. This list however does not imply an order of implementation; these activities must be carried out simultaneously by different teams, in efficient coordination.
a) Isolate the CTC and organize the sectors
- Demarcate the outer boundaries of the CTC
To begin with, use barrier netting. This provisional measure is sufficient while waiting to build a fence that may take several days.
- Demarcate the sectors of the CTC
To begin with, use barrier netting. The first priority is to demarcate the zones forbidden to patients (clean zone, morgue and waste storage area), then the different treatment zones (triage, hospitalisation, etc.).
The barrier netting can later be replaced by permanent barriers, but this is not essential as long as the netting stays intact and patients respect it.
b) Set up the tents
- Put up patient tents
- It is usually not necessary to put up all the estimated number of patient tents. For example, for a CTC with a capacity of 100 beds, start by putting up 5 tents then add further tents as/when admissions increase.
- Number the tents.
- Set up a hand-washing point in front of each tent.
- In each tent install:
- A container with a tap for ORS (+ bucket underneath).
- A cholera bed (or chair) + 2 buckets per patient (1 for stools, 1 for vomit). See Appendix 13.
- Infusion stands or ropes tied above the beds to hang infusion bags.
- Put up one or two tents for stock
It is essential to put away in storage all articles essential for patient treatment: Ringer lactate (RL) and infusion materials, oral rehydration salts (ORS), cups, buckets, lamps, 120-litre containers, jerrycans, electric lamps, chlorine-releasing compounds.
- Put up a tent to isolate deceased patients
Mortality is often high at the beginning of an outbreak. For obvious psychological reasons, remove deceased patients which are near other patients as quickly as possible.
c) Install initial stocks
Pallets (for boxes of ORS and RL) and shelves (for drugs and medical supplies/equipement) should be set up as quickly as possible.
d) Provide potable water
Initially potable water must be provided at least for drinking, preparing ORS and hand-washing. Water must be chlorinated.
- If the site has a water supply system, check the free residual chlorine levels and adjust if necessary (Appendix 17).
- If there is no water supply system:
- Water needs to be supplied by water truck or a vehicle with a water bladder, then stored in one or several bladders (or, if not possible, in containers of 120 litres) in the clean zone.
- Water can be transported manually to the different sectors while waiting for a water distribution system to be set up.
e) Set up hand-washing points
- To begin with: a hand-washing point for each patient tent, one in the morgue and one in the clean zone for staff.
- Waste water can be collected in buckets and transported manually to an excreta pit until a waste water evacuation system is set up.
- Other hand-washing points (at the entrance and exit of the CTC) can be set up the next day if they cannot all be installed on the same day.
f) Provide lighting
Lighting is essential for the continuity and safety of night care. Install a generator and lightbulbs as soon as possible if an electricity network does not exist. Lighting is first installed in sectors where patients are treated, then in the rest of the CTC if it cannot all be done on the same day. If there is no lighting the first night, work can always be carried out using lamps (headlamps, torches, kerosene lamps, etc.) but this should not be for long.
g) Dig latrines
To begin with, dig at least an excreta pit (Appendix 14), various latrines (male/female) for mobile patients and 2 latrines (male/female) for staff in the clean zone.
h) Set up waste storage area
- While waiting to set up a proper waste treatment area, demarcate a protected site to store waste.
- For sharps, use a drum that will later be filled with cement.
In the following days
Finish or complete installations: potable water distribution system, latrines, hand-washing points, showers, laundry point, rainwater drainage, soakaway pits, grease traps, zone for preparing chlorine solutions, stock storage, morgue, changing rooms, waste treatment area, kitchen, permanent fencing, etc. until the entire CTC is completely functioning.
It is important to differentiate the potable (chlorinated) water distribution system from the evacuation of waste water system. In order to avoid the risk of contamination of potable water in the event of a leak, these networks must not overlap.
Install or complete signage to help the increasing number of patients, attendants and staff to get around and correctly use the facilities (Section 6.1.6).
Note: the decision to open a CTC that is not yet ‘finished’ (i.e. not all the installations are complete) is up to the medical coordinator who is responsible for the treatment provided. It is he/she who decides if the minimum requirements are in place to start providing treatment.
- (a)For the MSF kit, see the MSF kit catalogue.