2.1 Indication
Postpartum haemorrhage due to uterine atony, when uterotonics fail to control bleeding.
An intrauterine balloon is used to reduce intrauterine bleeding and avoid haemostasis hysterectomy.
In a BEmONC facility, an intrauterine balloon can be used to stabilize the patient before referring her to a CEmONC facility.
2.2 Contra-indications
- Uterine rupture
- Purulent infection of the vagina, cervix or uterus
2.3 Balloon catheter placement
- Assess the need for analgesia/anaesthesia.
- Apply antiseptic solution (10% povidone iodine) to the perineal area.
- Remove any blood clots from the uterus (uterine exploration).
- Insert a Foley catheter.
- Estimate the size of the uterus and record it (for monitoring).
- Insert a speculum. Insert the (uninflated) balloon into the uterus, either manually or with atraumatic forceps. Make sure that the entire balloon passes the internal cervical os.
- Inflate the balloon with sterile, room temperature 0.9% sodium chloride, until it can be seen in the cervix (typically, 250 to 300 ml, 500 ml maximum); record the volume used).
- Apply gentle traction to the catheter and tape the end to the patient's thigh.
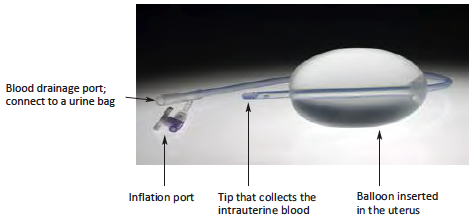
- Connect the drainage port to a fluid collecting bag (urine bag) to monitor haemostasis.
2.4 Associated treatment
- Continuous infusion of oxytocin: 20 to 40 IU depending on the dose already administered (max. 60 IU total dose) in 1 litre of Ringer lactate or 0.9% sodium chloride over 8 hours (42 drops/minute).
- Antibiotic treatment: ampicillin IV 1 g + metronidazole IV infusion 500 mg or amoxicillin/clavulanic acid IV (dose expressed in amoxicillin) 1 g, every 8 hours, until the balloon is removed.
- Start or continue blood transfusion to correct anaemia.
2.5 Patient follow-up
Hourly monitoring: vital signs, urine output, fundal height, vaginal bleeding, volume of blood collected in the collecting bag, SpO2 (if available).
If there is no blood flowing into the collection bag but the fundal height is increasing, the catheter may be blocked by clots: check to make sure it is open by instilling 15 to 30 ml of sterile 0.9% sodium chloride.
If there is no blood flowing into the collection bag, no vaginal flow, no increase in fundal height and the patient is stable, the bleeding is controlled: leave the balloon in place for 24 hours.
After 24 hours, remove half the injected volume from the balloon and check bleeding and vital signs after 30 minutes:
- If there is no visible bleeding and the patient is stable, completely deflate and remove the balloon.
- If the bleeding starts up again, re-inflate the balloon for another 6 to 8 hours and/or consider surgery.
If the initial tamponade fails or the bleeding starts again while the inflated balloon is still in place, surgical treatment is indicated.