1.2.1 Aims of antenatal monitoring
- Screening for and management of pathologies: hypertension, anaemia, malaria, syphilis, urinary tract infection, HIV infection, malnutrition, vitamin and micronutrient deficiencies, etc.
- Screening for and management of obstetric complications: uterine scar, abnormal presentation, premature rupture of membranes, multiple pregnancy, abnormal bleeding (metrorrhagia), etc.
- Routine prevention of maternal and neonatal tetanus, anaemia, mother-to-child HIV transmission, malaria in endemic areas, etc.
- Devising a birth plan; counselling; preparation for the birth.
1.2.2 Timing of antenatal consultations
Four antenatal consultations are recommended for uncomplicated pregnancies.
If the woman does not come in until the sixth month or later, try to have at least 2 consultations before the birth.
Table 1.2 - Schedule of antenatal consultations
| Trimester | Month | Weeks LMP (a)Citation a.The gestational age is expressed in weeks since last menstrual period (LMP) or, less precisely, in months of pregnancy. Pregnancy lasts 9 months or 40 or 41 weeks LMP, depending on the country. | Consultation schedule |
|---|---|---|---|
First | 1 2 3 | 2-5 6-9 10-13 |
<= Consultation 1 |
Second | 4 5 6 | 14-17 18-21 22-26 | <= Consultation 2 |
Third | 7 8 9 | 27-30 31-35 36-40/41 | <= Consultation 3
<= Consultation 4 |
Closer monitoring may be needed, depending on the problems detected and the patient’s history (Section 1.3).
1.2.3 First consultation
A. History taking
- General feeling about the pregnancy (problems/concerns).
- Social context: family situation, screening for sexual, intimate partner and domestic violence, living conditions, professional activity, etc.
- Date of last menstrual period.
- Obstetric and surgical history:
- Number of prior pregnancies;
- Complications during prior pregnancies/deliveries (haemorrhage, infection, prematurity, etc.);
- Spontaneous or induced abortion(s);
- Children, alive and deceased;
- Caesarean section (find out why) or any other uterine surgery;
- Instrumental delivery;
- Vesicovaginal or rectovaginal fistula;
- Medical history and ongoing treatments: hypertension, diabetes, asthma, epilepsy, heart disease, HIV infection, psychiatric disorder, etc.;
- Tetanus immunisation status;
- Current complaints: pelvic pain, contractions, fever, urinary symptoms, vaginal bleeding, abnormal vaginal discharge, etc.
B. Estimating the gestational age and due date
The gestational age is estimated by counting the number of weeks since the last menstrual period (weeks LMP) using a calendar or pregnancy wheel.
For example, if the last menstrual period was on 15 December 2018 and the woman is seen on 27 January 2019, the estimated gestational age is 6 weeks LMP.
Always verify that this estimate tallies with the data from the clinical examination (estimate of uterine size) or the ultrasound.
The due date is estimated by counting 40 or 41 weeks from the first day of the last menstrual period. For example, if the date of the last menstrual period was 15 December 2018, the due date is between 22 and 29 September 2019.
The due date can also be estimated by counting 9 months plus 7 to 14 days from the first day of the last menstrual period.
If the woman does not know the date of her last menstrual period, the presumed gestational age and due date is determined based on clinical examination or ultrasound if available
aCitation a.Ultrasound allows accurate estimation of gestational age in the first trimester, with a margin of error of approximately 7 days. The margin of error is larger in the second and third trimesters (about 15 and 20 days, respectively).
.
C. Clinical examination
In all cases:
- Weight
- Height (detection of women < 1.50 m)
- Blood pressure (patient seated and resting)
- Look for abdominal scar.
- Look for anaemia, oedema, etc.
- Look for foetal heart tones after the end of the first trimester.
- Estimate the size of the uterus (gives an estimate of gestational age):
- during the first trimester, the size of the uterus is estimated by bimanual examination. At 7 weeks the uterus is the size of a chicken egg, at 10 weeks the size of an orange, and at 12 weeks the uterine fundus extends beyond the symphysis pubis;
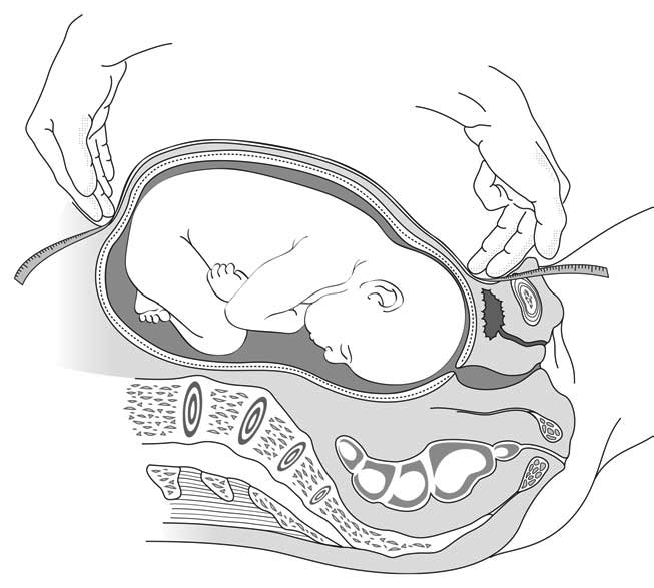
- from the beginning of the second trimester, the uterus can be felt by abdominal palpation alone; measure the fundal height, which is the distance between the upper edge of the symphysis pubis and the fundus (Figure 1.1).
Figure 1.1 - Measuring the fundal height
Estimation of gestational age becomes increasingly approximate as the pregnancy progresses. As a rough guide:
Table 1.3 - Fundal height according to gestational age
| Fundal height | Weeks since last menstrual period |
|---|---|
| 20 cm | 18 - 22 weeks LMP |
| 24 cm | 22 - 26 weeks LMP |
| 28 cm | 26 - 30 weeks LMP |
| 32 cm | 30 - 34 weeks LMP |
| 34 cm | 33 weeks LMP to term |
Note: fundal height and uterine growth may vary with ethnicity. Use the national curves from the Ministry of Health, if they exist.
Only if indicated:
- Genital examination (e.g. to look for mutilation, symptoms of sexually transmitted infection).
- Vaginal examination (e.g. if there is doubt about the pregnancy diagnosis).
D. Laboratory tests
Table 1.4 - Recommended screening tests
| Tests | Comments |
|---|---|
| Syphilis | Syphilis screening should be performed at the first consultation, as early as possible in pregnancy. If the initial test is negative, re-testing is recommended as of 28 weeks LMP for women at high risk of infection or if syphilis prevalence is ≥ 5% [1]Citation 1.World Health Organization. WHO Antenatal Care Randomised Trial: Manual for the Implementation of the New Model. Geneva. 2002. WHO/RHR/01.30. http://whqlibdoc.who.int/hq/2001/WHO_RHR_01.30.pdf . If it was not performed during an antenatal consultation, the test should be performed at delivery. Use a treponema-specific rapid test (e.g., SD Bioline®). |
| Malaria | In endemic areas, perform a rapid test even if there are no symptoms. |
| HIV infection | Offer a test to all women who do not know their HIV status. Perform rapid tests according to the standard algorithm. Testing cannot be peformed without the patient’s consent. If it was not performed during an antenatal consultation, it should be performed at delivery. If possible, evaluate the immunological status (CD4 count) if seropositivity is detected, or at the first antenatal consultation for women who already know that they are HIV positive. |
| Anaemia | Measure haemoglobin (HemoCue). Hb levels defining anaemia are < 11 g/dl (first and third trimester) and < 10.5 g/dl (second trimester). If it was not measured during an antenatal consultation, it should be measured at delivery. |
| Urinary tract infection | Test for asymptomatic bacteriuria, even if there are no symptoms (urinalysis with reagent test strips). |
E. Antenatal care card
Fill out all relevant information on an individual antenatal care card to monitor the progress of the pregnancy (Appendix 1).
1.2.4 Subsequent consultations
A. History taking
- Foetal movement felt by the mother.
- Current complaints: pelvic pain, contractions, fever, urinary symptoms, vaginal bleeding, abnormal vaginal discharge, etc.
B. Clinical examination
Be careful when examining a woman lying on her back; the weight of the uterus compresses the inferior vena cava, which can cause her to feel faint (easily remedied by placing the patient on her left side).
In all cases:
- Blood pressure, weight, oedema, fundal height.
- Foetal heart tones: should be regular, rapid (110-160/minute), and out of sync with the mother’s pulse.
- Foetal presentation (third trimester):
Palpation:- Cephalic pole: round, hard and regular; there should be a feeling of ballottement between examiner’s hands; separated from the rest of the body by the indentation of the neck, beyond which the projection of the shoulder can be palpated.
- Pelvic pole: soft; bulkier and less regular than the cephalic pole; no neck indentation.
Types of presentation:
Cephalic: the cephalic pole points towards the mother’s pelvis.
Breech: the cephalic pole is in the uterine fundus.
Transverse: the poles lie in each of the mother’s sides.
Exploring the foetal back:
Press the uterine fundus downward to bend the foetal spine and explore the lateral surfaces of the uterus. The back is felt as a hard plane, the limbs as small irregular projections. The back is described with reference to the mother’s right or left.In the third trimester, the foetal heart tones are auscultated in the umbilical region along the foetus’ back, at shoulder level.
Only if indicated:
- Genital examination (e.g. to look for symptoms of sexually transmitted infection).
- Vaginal examination (e.g. if mother complains of recurring uterine contractions).
Note: a small pelvis bCitation b.The pelvis is considered small if the top of the sacrum (promontory) can be reached with the fingers and/or the lateral edges of the pelvis can be felt along their entire length. is not predictive of foeto-pelvic disproportion and does not justify scheduling a caesarean section. Moreover, foeto-pelvic disproportion can occur with a normal-appearing pelvis. In practice, foeto-pelvic disproportion can only be diagnosed during labour.
C. Laboratory tests
Table 1.5 - Recommended screening tests
| Tests | Comments |
|---|---|
| Urinary tract infection | Look for asymptomatic bacteriuria at each consultation. |
| Malaria | In endemic areas, perform a rapid test at each consultation during the second and third trimesters, unless the woman was tested in the past 4 weeks, the test was positive, and the woman has taken curative antimalarial treatment as a result. |
| HIV infection | Offer patients who tested negative during the first trimester a new test in the third trimester. There is increased risk of mother-to-child transmission of HIV when seroconversion occurs during pregnancy. |
1.2.5 Preventive treatments
Maternal and neonatal tetanus
- Pregnant women not vaccinated against tetanus in childhood or adolescence should receive at least 2 doses of tetanus vaccine (TV)
cCitation c.Use preferably Td vaccine (tetanus and diphtheria toxoids) or, if not available, TT vaccine (tetanus toxoid).
before giving birth:
- the first dose should be administered at the first consultation;
- the second dose should be administered at least 4 weeks after the first dose and ideally at least 2 weeks before the due date to maximize the maternal antibody response and passive antibody transfer to the infant.
- After the birth, continue to a total of 5 doses, according to the schedule below. Once administered, these 5 doses confer lifelong protection.
Table 1.6 - Vaccination schedule for women who are pregnant or of child-bearing age
[2]Citation 2.World Health Organization. Field manual for neonatal tetanus elimination. Geneva. 1999.
http://whqlibdoc.who.int/hq/1999/WHO_V&B_99.14.pdf
| Dose | Schedule | Level of protection |
|---|---|---|
| TV1 | At the first contact with medical services or as early as possible during pregnancy | 0% |
| TV2 | At least 4 weeks after TV1 and at least 2 weeks before the delivery due date | 80% |
| TV3 | At least 6 months after TV2 or during the next pregnancy | 95% |
| TV4 | At least 1 year after TV3 or during another pregnancy | 99% |
| TV5 | At least 1 year after TV4 or during another pregnancy | 99% |
Anaemia
Absence of anaemia
If there are no clinical signs of anaemia and no abnormal haemoglobin values:
- Administer iron and folic acid supplementation, starting as soon as possible after gestation starts and continue throughout the rest of the pregnancy. Give either:
ferrous sulfate/folic acid dCitation d.200 mg ferrous sulfate (65 mg elemental iron) + 400 micrograms folic acid tablets may be replaced by 185 mg ferrous fumarate (60 mg elemental iron) + 400 micrograms folic acid tablets. (tablet containing 200 mg of ferrous sulfate, 65 mg of elemental iron + 400 micrograms of folic acid) PO: 1 tablet once daily
or
multiple micronutrients eCitation e.If using multiple micronutrients, check the amount of iron salts (sulfate or fumarate) is equivalent to 30 mg of elemental iron per tablet and the amount of folic acid is 400 micrograms per tablet (UNU/UNICEF/WHO formulation). (tablet containing 93.75 mg of ferrous sulfate, equivalent to 30 mg of elemental iron + 400 micrograms of folic acid + other nutrients) PO: 1 tablet once daily
Note: World Health Organization recommends 30 to 60 mg of elemental iron daily. However, a dose of 60 mg of elemental iron daily is preferred over a dose of 30 mg daily in settings where the prevalence of anaemia in pregnant women is high (≥ 40%) fCitation f.According to the World Health Organization (1993-2005), the prevalence of anaemia in pregnant women is 57.1% in Africa, 48.2% in South-East Asia, 44.2% in the Eastern Mediterranean region, 30.7% in the Western Pacific region, 25% in the European region and 24.1% in the Americas., [3]Citation 3.World Health Organization. Guideline: Daily iron and folic acid supplementation in pregnant women. Geneva. 2012.
http://apps.who.int/iris/bitstream/10665/77770/1/9789241501996_eng.pdf . - In areas where hookworm infection is common (areas with warm, moist climates), administer also an antihelminthic treatment as of the second trimester:
albendazole PO, 400 mg single dose (or mebendazole PO: 100 mg 2 times daily for 3 days) - In areas where malaria is endemic, administer also an intermittent preventive antimalarial treatment or an antimalarial curative treatment, depending on the results of malaria screening tests (see below).
Presence of anaemia
If there is clinical evidence of anaemia (pallor of the palms, conjunctivae or tongue) or if haemoglobin is < 11 g/dl in the first and third trimester or < 10.5 g/dl in the second trimester): see Chapter 4, Section 4.1.
Malaria
In all areas with moderate to high P. falciparum malaria transmission gCitation g.“Moderate transmission” areas: zones where prevalence rate of malaria is 11 to 50% during most of the year among children aged 2 to 9 years. “High transmission” areas: zones where prevalence rate of malaria is over 50% during most of the year among children aged 2 to 9 years. prevention consists of:
- The use of insecticide-treated mosquito nets (2 bed nets should be provided).
- Malaria testing at each antenatal consultation in the second and third trimesters.
- If the test is positive, no matter the region or stage of pregnancy:
Administer curative malaria treatment (Chapter 4, Section 4.3.1).
Wait one month after curative treatment before screening for malaria again. - If the test is negative, intermittent preventive treatment (IPT) is recommended in African moderate to high P. falciparum malaria transmission areas:
Start IPT with sulfadoxine-pyrimethamine (SP) [4]Citation 4.WHO policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP). April 2013 (revised January 2014).
http://www.who.int/malaria/publications/atoz/iptp-sp-updated-policy-brief-24jan2014.pdf as early as possible in the second trimester. The aim is to administer at least 3 doses between the second trimester and delivery with an interval of at least 1 month between each treatment. There is no maximum number of treatments as long as a one-month interval is respected. The SP dose for each treatment is 3 tablets single dose. This treatment helps reduce the effects of malaria (maternal anaemia and low birth weight). Do not administer this intermittent treatment to HIV-infected women receiving co-trimoxazole prophylaxis.
- If the test is positive, no matter the region or stage of pregnancy:
Urinary tract infections
Treat all urinary tract infections including asymptomatic bacteriuria
[5]Citation 5.Smaill F, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy (Review). The Cochrane Library 2007, Issue 4.
http://apps.who.int/rhl/reviews/CD000490.pdf
detected by urine dipstick test (Chapter 4, Section 4.2.3).
HIV infection
If test results are positive, start antiretroviral therapy (Chapter 4, Section 4.4.4).
Vitamin and micronutrient deficiencies
- Calcium
Supplementation is recommended for [6]Citation 6.World Health Organization. WHO recommendations on antenatal care for positive pregnancy experience. 2016.
https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf;jsessionid=011FCED838D9A9884D9D1FC1285B16FB?sequence=1 :- All pregnant adolescents (under 20 years old);
- All pregnant women with low calcium intake AND at high risk of pre-eclampsia (history of pre-eclampsia or eclampsia, twin pregnancy, chronic hypertension).
Start supplementation at the first antenatal visit and continue throughout the pregnancy:
calcium carbonate PO: one 1.25 g tablet (equivalent to 500 mg of calcium element) 3 times daily
Wait 2 hours between the administration of calcium and ferrous salts.
- Vitamin D
Sun exposure and foods are sources of vitamin D. A supplement can be prescribed if there is a risk of deficiency (low exposure to sunlight, diet poor in vitamin D):
colecalciferol (vitamin D3) or ergocalciferol (vitamin D2) PO: 100 000 IU single dose at 6 or 7 months of pregnancy. - Iodine
Iodine deficiency during pregnancy increases the risk of miscarriage, prematurity, severe mental and growth restriction in the child, and neonatal or infant death. In areas where iodine deficiency is endemic, iodine supplementation is necessary. Follow national protocol.
Malnutrition
- If malnutrition is present, admit the woman into a therapeutic feeding programme. If there no therapeutic feeding programme, ensure supplementation:
- MUAC 190-230 mm: 2 sachets Plumpy'nut or 3 bars BP100 daily;
- MUAC < 190 mm: 4 sachets Plumpy'nut or 7 bars BP100 daily.
- In the absence of signs of malnutrition but in a context of food insecurity, food supplementation is recommended for all pregnant women throughout their pregnancy.
- In the event of overweight or obesity, provide advice on how to avoid excessive weight gain during pregnancy.
| The above measures apply to most contexts. Other tests and preventive measures relevant in the specific context , or included in the national protocol (e.g. Rhesus factor testing and alloimmunization prophylaxis, screening for cervical cancer, hepatitis B serology, screening for tuberculosis, etc.), should be taken into account. |
1.2.6 Preparation for the birth
Group sessions
Group sessions (10 to 15 women) should be organized to encourage information sharing between patients, promote the use of available services and address the following:
- Importance of skilled birth assistance.
- The purpose of antenatal consultations.
- The recommended screening tests and preventive treatments during pregnancy.
- Protection against insect vectors: insecticide-treated mosquito nets, protective clothing, certain repellents, etc. according to the context (e.g. malaria, dengue, chikungunya, zika).
- Danger signs during pregnancy, labour and delivery, and the importance of quickly seeking medical care.
- The use of the “birth kit” hCitation h.Individual kit given to women that might deliver at home due to limited travel possibility (remote or insecure situations). It contains a plastic-coated cloth to be spread out on the floor, a soap (for cleaning the woman’s genitals and washing the midwife’s hands), a string and a razor blade for tying and cutting the cord and, in some cases, a cloth for drying the infant. , depending on the context.
- The purpose of the postnatal consultation.
- Contraception.
Individual sessions
Individual sessions are an opportunity to revisit the subjects discussed in the group sessions and offer advice tailored to the individual's medical and social situation.
The choice of topics depends on the stage of pregnancy and the woman’s specific circumstances (e.g. substance abuse, domestic violence, genital mutilation).
Individual sessions should in all cases include a personalised birth plan (see below).
Birth plan
With the patient, work out a plan appropriate to her medical and social situation:
- Site for birth: BEmONC or CEmONC facility, depending on the course of the pregnancy and the history;
- Any necessary arrangements: transportation, family arrangements, etc.
Table 1.7 - Obstetric care facilities
| Facility | Minimum package |
|---|---|
| BEmONC Basic Emergency Obstetric and Newborn Care |
|
| CEmONC Comprehensive Emergency Obstetric and Newborn Care |
|
- (a)Ultrasound allows accurate estimation of gestational age in the first trimester, with a margin of error of approximately 7 days. The margin of error is larger in the second and third trimesters (about 15 and 20 days, respectively).
- (b)The pelvis is considered small if the top of the sacrum (promontory) can be reached with the fingers and/or the lateral edges of the pelvis can be felt along their entire length.
- (c)Use preferably Td vaccine (tetanus and diphtheria toxoids) or, if not available, TT vaccine (tetanus toxoid).
- (d)200 mg ferrous sulfate (65 mg elemental iron) + 400 micrograms folic acid tablets may be replaced by 185 mg ferrous fumarate (60 mg elemental iron) + 400 micrograms folic acid tablets.
- (e)If using multiple micronutrients, check the amount of iron salts (sulfate or fumarate) is equivalent to 30 mg of elemental iron per tablet and the amount of folic acid is 400 micrograms per tablet (UNU/UNICEF/WHO formulation).
- (f)According to the World Health Organization (1993-2005), the prevalence of anaemia in pregnant women is 57.1% in Africa, 48.2% in South-East Asia, 44.2% in the Eastern Mediterranean region, 30.7% in the Western Pacific region, 25% in the European region and 24.1% in the Americas.
- (g)“Moderate transmission” areas: zones where prevalence rate of malaria is 11 to 50% during most of the year among children aged 2 to 9 years. “High transmission” areas: zones where prevalence rate of malaria is over 50% during most of the year among children aged 2 to 9 years.
- (h)Individual kit given to women that might deliver at home due to limited travel possibility (remote or insecure situations). It contains a plastic-coated cloth to be spread out on the floor, a soap (for cleaning the woman’s genitals and washing the midwife’s hands), a string and a razor blade for tying and cutting the cord and, in some cases, a cloth for drying the infant.
- aThe gestational age is expressed in weeks since last menstrual period (LMP) or, less precisely, in months of pregnancy. Pregnancy lasts 9 months or 40 or 41 weeks LMP, depending on the country.
- 1.World Health Organization. WHO Antenatal Care Randomised Trial: Manual for the Implementation of the New Model. Geneva. 2002. WHO/RHR/01.30.
http://whqlibdoc.who.int/hq/2001/WHO_RHR_01.30.pdf - 2.World Health Organization. Field manual for neonatal tetanus elimination. Geneva. 1999.
http://whqlibdoc.who.int/hq/1999/WHO_V&B_99.14.pdf - 3.World Health Organization. Guideline: Daily iron and folic acid supplementation in pregnant women. Geneva. 2012.
http://apps.who.int/iris/bitstream/10665/77770/1/9789241501996_eng.pdf - 4.WHO policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP). April 2013 (revised January 2014).
http://www.who.int/malaria/publications/atoz/iptp-sp-updated-policy-brief-24jan2014.pdf - 5.Smaill F, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy (Review). The Cochrane Library 2007, Issue 4.
http://apps.who.int/rhl/reviews/CD000490.pdf - 6.World Health Organization. WHO recommendations on antenatal care for positive pregnancy experience. 2016.
https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf;jsessionid=011FCED838D9A9884D9D1FC1285B16FB?sequence=1