5.2.1 Diagnosis and sorting
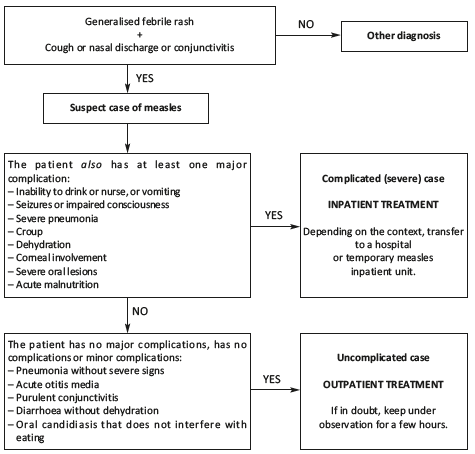
Look for clinical signs of measles, and determine whether the patient is a “complicated case” or an “uncomplicated case”.
5.2.2 Initial clinical examination
Confirm the measles diagnosis
The rash consists of non pruritic small red or pink spots (macules) that are separated by areas of healthy skin and blanch under pressure.
The patient also has a cough and/or runny nose and/or eye discharge.
Measure the axillary temperature or, at a minimum, verify that the child feels "hot”. The fever is generally high (> 39 °C).
Look for respiratory complications
Check that the child is breathing normally, and is not congested or dyspnoeic.
In case of nasal obstruction (common), clear the nasopharynx.
If he is coughing or dyspnoeic, measure the respiratory rate (RR). Auscultate the patient, if possible, depending on the examiner’s skills.
Using the following criteria, hospitalise children with severe pneumonia. Uncomplicated pneumonia with no severity criteria can be treated on an outpatient basis, if the child is not a “complicated case” for other reasons.
|
Pneumonia (no severe signs) |
Severe pneumonia |
|---|---|
|
Fever and cough |
Signs of pneumonia
|
Hospitalise any children with stridor (mild to moderate or severe croup).
Look for otitis
Look for ear pain and purulent discharge from the auditory canal. Perform an otoscopic examination, if possible, depending on the examiner’s skill.
Otitis can be treated on an outpatient basis, if the child is not a “complicated case” for other reasons.
Look for ocular complications
Clean the eye beforehand if copious secretions interfere with the examination. Examine each eye separately, using a flashlight. Examine the conjunctiva and cornea. Determine whether there is corneal involvement or not. Proceed with care as corneal lesions are often painful and accompanied by photophobia (the patient shields his eyes from the light).
The normal cornea is transparent (it allows a clear view of the iris and pupil), moist, and shiny (it reflects the light). Any abnormality: loss of transparency (opacity) or shininess (dull or dry cornea), or corneal softening (necrosis, perforation) is an indication for hospitalisation (= complicated case).
Purulent conjunctivitis by itself (purulent discharge with discomfort or foreign body sensation, without photophobia nor corneal involvement) can be treated on an outpatient basis, if the child is not a “complicated case” for other reasons.
The examination can show Bitot’s spots, which are foamy, whitish patches on the bulbar conjunctiva (white of the eye). The child can be treated on an outpatient basis if he is not a "complicated case" for other reasons.
Look for oral lesions
Oral candidiasis (white patches on the tongue or within the oral cavity) is considered benign unless it prevents eating. It can be treated on an outpatient basis, if the child is not a“complicated case” for other reasons.
Painful or extensive lesions that prevent children from drinking or eating are all considered severe (= complicated case).
Look for dehydration and/or diarrhoea
In patients with diarrhoea, look for dehydration.
Look for dehydration in children even if there is no diarrhoea. They can be dehydrated for other reasons (e.g. insufficient fluid intake, repeated vomiting, or high fever).
No matter what the cause, patients who are dehydrated must be hospitalised (= complicated case).
Weight
Weight the child whenever possible.
Ability to drink
Put the child to the breast or offer him water to make sure that he drinks/eats.
Nutritional status
Look for malnutrition only if justified by the context (food insecurity or crisis, or displaced population) and in children under age 3 or 5 years.
First look for bilateral lower extremity oedema:
- if there is bilateral oedema: acute malnutrition (= complicated case);
- if there is no bilateral oedema, measure the mid-upper arm circumference (MUAC):
- if MUAC > 125 mm: the child is not malnourished;
- if MUAC ≤ 125 mm, weigh and measure the child to calculate the weight-for-height ratio (W/H). If the W/H ratio is < –2 standard deviation: acute malnutrition (= complicated case);
- if MUAC < 115 mm: severe acute malnutrition (= complicated case).
- (a)In children with severe malnutrition, reduce these thresholds by 5.