10% of neonates need help breathing properly at birth; this help comes in the form of tactile stimulation and/or airway clearing.
For half of them, these procedures are not sufficient, and if the neonate is not breathing or is gasping despite stimulation/suction, ventilation is needed as of the first minute of life.
A small percentage of ventilated newborns will require more advanced resuscitation.
The birth attendant in charge of the delivery is also responsible for the newborn. S/he should start resuscitation immediately then, if necessary, call for help.
10.2.1 Basic resuscitation aCitation a.For more information, refer to the Helping Babies Breathe training course.
Steps 1 to 5 should be performed in the first minute of life. Record all procedures on the monitoring sheet.
1 - Stimulate the neonate by drying
Tactile stimulation can trigger spontaneous breathing. It is done by drying the neonate.
If the neonate starts to breathe or cry within 5 seconds, proceed to routine care (Section 10.1).
If not, stop stimulation and proceed to step 2.
2 - Clear the airway
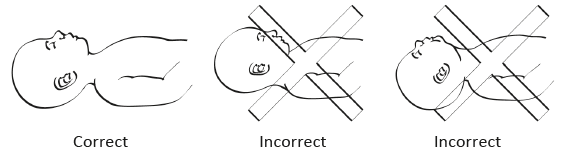
Lay the neonate on the back with the head in a neutral position (Figure 10.1); avoid flexion or hyperextension of the neck, as this can obstruct the airway.
Figure 10.1 - Head position for clearing the airway
Only in cases where there are copious secretions, suction the mouth gently i.e., not too deeply (maximum depth 2 cm from the lips) – and quickly (maximum duration 5 seconds) with a bulb syringe.
If neonate is still not breathing or not breathing well, proceed to step 3.
3 - Stimulate the neonate
Rub the back and the soles of the feet vigorously but not roughly (do not shake, slap or hang the infant by the feet, etc.). If the neonate is having difficulty breathing or still not breathing after 5 seconds: stop active stimulation, and proceed to steps 4 and 5.
4 - Clamp and cut the cord
If not already done, clamp and cut the cord.
5 - Perform bag-mask ventilation (room air)
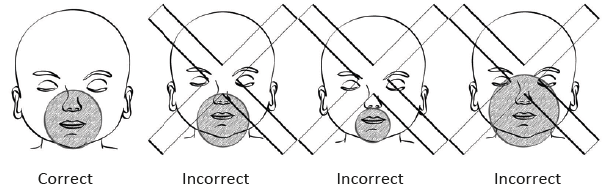
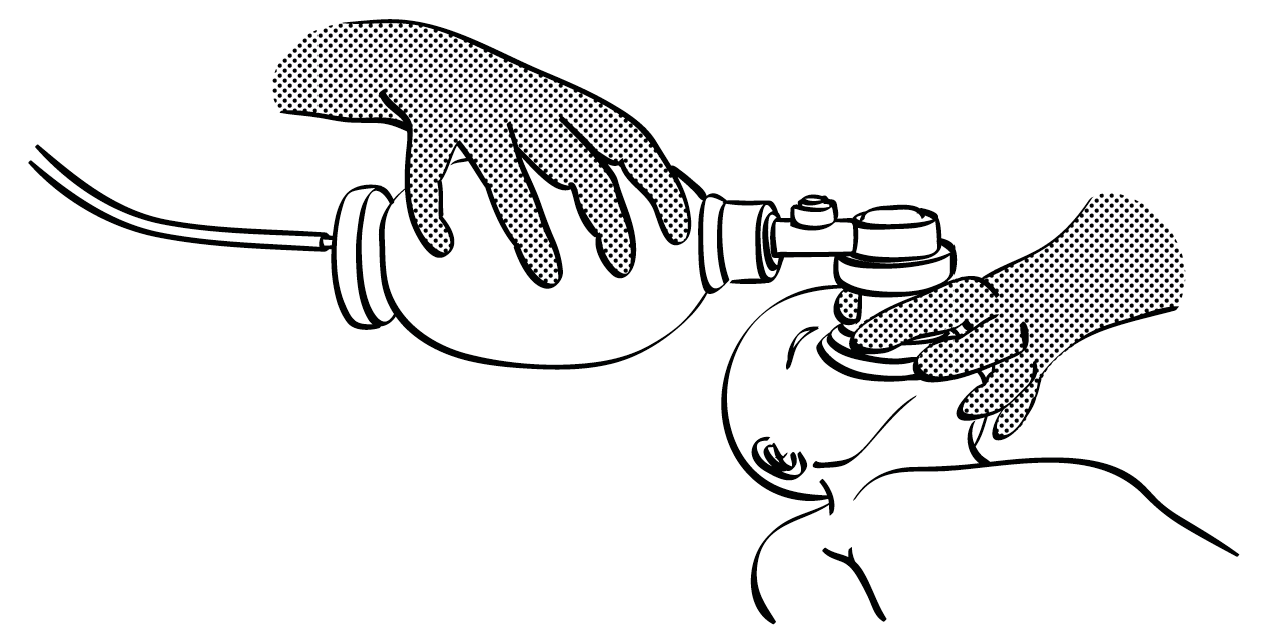
- Fit the mask over the nose and mouth. Press firmly to prevent air leaks. Hold it with one hand, with the thumb on one side and the index and middle fingers on the other (Figures 10.2 and 10.3). With the other hand, squeeze the bag at a rate of 30 to 60 breaths/minute for 60 seconds. Ventilation is effective if the chest rises and falls.
Attention, excessive ventilation pressure can cause a pneumothorax.
- If the chest fails to rise:
- Check the connection between the bag and the mask;
- Correct the position of the mask on the face;
- Correct the head position.
Figure 10.2 - Mask position
Figure 10.3 - Manual ventilation
- Check every minute for spontaneous respiratory effort (look for chest movement); do not take the mask off the neonate’s face to check for spontaneous breathing.
- Continue manual ventilation until there is spontaneous respiratory effort.
6 - Oxygenation
If oxygen is available: connect the ambu bag to an oxygen reservoir after 2 minutes of ventilation, setting it at a 2 litres/minute flow rate. Ventilation is a priority and should not be interrupted to connect the oxygen (have an assistant connect the oxygen).
Stop resuscitation if the neonate has:
- No heart rate after 10 minutes.
- No spontaneous respiration after 20 minutes of effective ventilation, even if the heart rate is adequate.
10.2.2 After resuscitation
- Re-evaluate all vital signs, look for danger signs and measure blood glucose. Perform a retroactive Apgar score assessment (Section 10.1.1).
- Record the results on a monitoring sheet.
- Transfer to a neonatal care unit is indicated if one of the following is present:
- The neonate was ventilated with a mask for 2 minutes or more.
- The Apgar score was ≤ 4 at 1 minute or ≤ 6 at 5 minutes.
- Any danger sign is present (Section 10.3.1).
- Keep the mother and neonate together where possible.
- If the neonate appears well (no indications for transfer) or if transfer is necessary but impossible:
- Keep under observation for at least 24 hours.
- Every 2 hours, check for any danger signs (Section 10.3.1) and monitor vital signs.
- Ensure routine care (Section 10.1).
- Begin breastfeeding as soon as possible.
- If the neonate deteriorates during close observation, refer to Section 10.3 for further management.
- (a)For more information, refer to the Helping Babies Breathe training course.