Low birth weight indicates prematurity (less than 37 weeks) or intrauterine growth restriction or a combination of the two.
Low birth weight neonates, whether preterm or not, are at significant short-term risk of hypothermia, hypoglycaemia, apnoea, respiratory distress, jaundice, infection, anaemia, dehydration and feeding problems, and at significant long-term risk of poor psychomotor development.
Neonates who are sick or who weigh less than 1500 g should be referred to a neonatal care unit whenever possible.
Neonates who weigh 1500 to 2500 g, regardless of the term, are managed in the maternity hospital if they are not sick, according to the recommendations below.
10.5.1 Kangaroo care
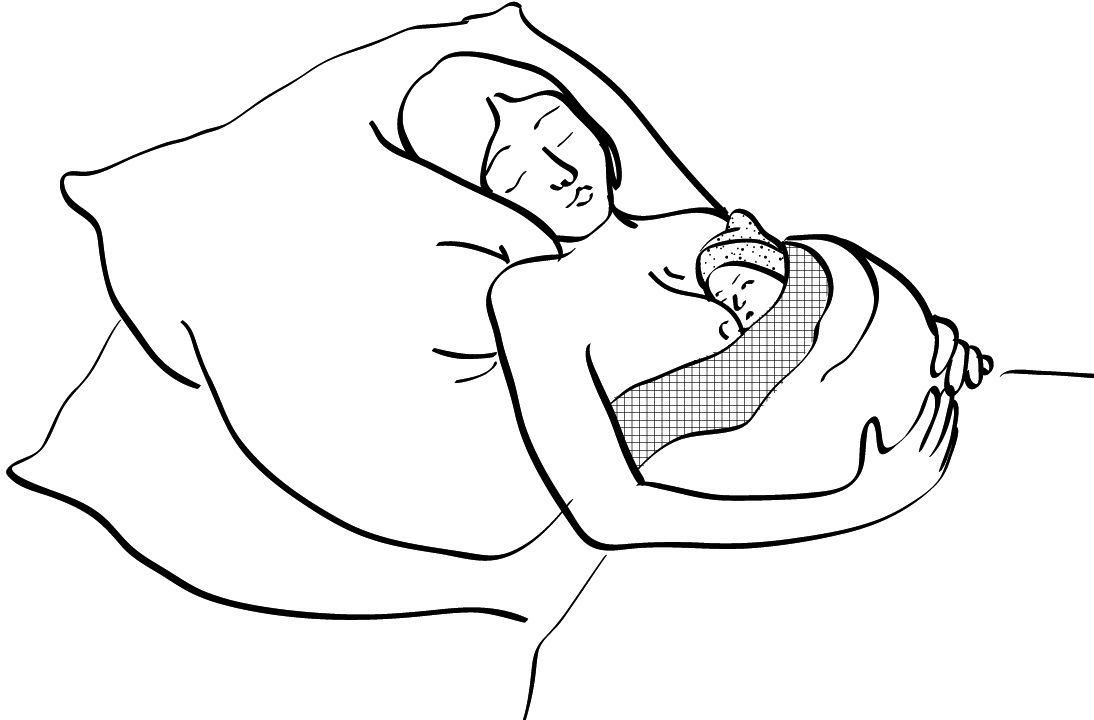
Figures 10.4 - Kangaroo care
 |
 |
The Kangaroo mother care
aCitation a.For more information: World Health Organization. Kangaroo mother care: a practical guide. 2003.
http://apps.who.int/iris/bitstream/handle/10665/42587/9241590351.pdf?sequence=1
is a method of caring for neonates that involves putting them on the mother's chest skin-to-skin, preferably 24 hours a day.
This method can be used for all non-sick neonates less than 2500 g (prematurity and/or intrauterine growth restriction).
The neonate is placed vertically against the mother’s chest (may wear nappy and socks); the mouth should always be able to reach the nipple. Keep the neonate in position using a cloth.
If needed, use a blanket to keep the mother and neonate warm.
When the mother is sleeping, her bust should be raised and the neonate should be monitored.
The objectives of the Kangaroo care are:
- To keep the neonate warm and to prevent or treat hypothermia.
- To help get breastfeeding started and keep it going.
- To foster the mother-infant bond and reduce the neonate’s stress.
- To reduce episodes of apnoea and bradycardia in preterm neonates.
Note: the skin-to-skin contact can also be done by the father, another family member or a wet-nurse during periods when the mother is not available.
10.5.2 Thermoregulation
- Cover the neonate’s head to reduce heat loss.
- Make sure that the room temperature is between 23-25 °C.
- Use the Kangaroo care (Section 10.5.1).
10.5.3 Feeding
- Exclusive breastfeeding is the best choice (Appendix 3).
- If sucking is ineffective but the swallowing reflex is present, express the milk manually or using a breast pump and feed the neonate using a cup/spoon (Appendix 3, Section 3.2 and Section 3.3).
- If sucking is ineffective and the swallowing reflex is poor or absent, express the milk and feed the neonate using a gastric tube (Appendix 3, Section 3.2 and Section 3.4).
- For the daily amounts required for feeding, see Appendix 4.
- If the mother does not have enough milk:
- In the first 72 hours of life, make up the required amounts with 10% glucose PO.
- After 72 hours of life, make up the amount with infant formula (or if not available, use diluted F 100 milk bCitation b.Diluted F-100 milk: 1 sachet (456 g) of F-100 milk in 2800 ml of water. ).
- At the same time, continue to stimulate the mother’s milk production (breast pump and the “supplementary nursing" technique, Appendix 3, Section 3.5).
- In all cases, try putting the neonate to the breast periodically to test if breastfeeding is effective or not.
- In the event of regurgitation:
- Administer each meal very slowly.
- Hold the neonate tilted slightly head-up.
- In the event of vomiting, abdominal distension, blood in the stool or greenish, foul-smelling stool, stop feeding and call the doctor immediately.
- Very low birth weight neonates (< 1500 g) have a high risk of developing acute necrotising enterocolitis with early oral feeding. For the first 48 hours, give a 10% glucose IV continuous infusion (Appendix 5). If the neonate is clinically stable, very small amounts of breast milk of 10 ml/kg per day can be started on D1 while awaiting transfer to a neonatal care unit.
- If it is not possible to administer an IV infusion or to transfer to a neonatal care unit, give expressed breast milk and 10% glucose together orally (Appendix 4).
10.5.4 Monitoring
Same monitoring as for a neonate > 2500 g, plus:
- Daily weighing;
- Temperature every 4 hours;
- Blood glucose test before every meal or every 3 hours until there are 3 consecutive normal results. In the event of hypoglycaemia, see Section 10.3.4.
- (a)For more information: World Health Organization. Kangaroo mother care: a practical guide. 2003.
http://apps.who.int/iris/bitstream/handle/10665/42587/9241590351.pdf?sequence=1 - (b)Diluted F-100 milk: 1 sachet (456 g) of F-100 milk in 2800 ml of water.