Contenido
Partial incision of the cartilage of the symphysis pubis such that the two pubic bones separate by about 2 cm, allowing enough room for passage of an entrapped, live foetus.
This procedure should be done in combination with episiotomy (Section 5.8) and instrumental delivery (Section 5.6).
5.7.1 Indications
This life-saving technique may be useful as a procedure of last resort:
- In situations where caesarean section is indicated but not feasible
aCitation a.Caesarean section is not feasible because surgical conditions are inadequate or surgical intervention would take too long or there is a high risk of trauma to mother and foetus or the woman refuses caesarean section.
:
- Head engaged and arrested for more than an hour, and vacuum extraction alone has already failed or is likely to do so.
- Foeto-maternal disproportion due to a pelvis that is slightly too narrow: after the trial of labour has failed, and at least 3/5 of the head has descended into the pelvic cavity.
- In the event of shoulder dystocia when other manoeuvres have failed.
- In the event of entrapped aftercoming head in a breech when other manoeuvres have failed.
5.7.2 Conditions
- Membranes ruptured, full dilation.
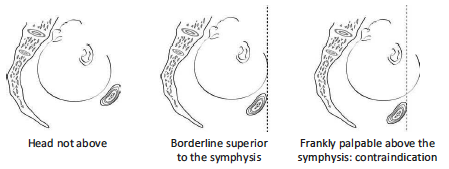
- The foetal head is not palpable above the symphysis pubis or by less than 2/5 (Figure 5.17).
5.7.3 Contra-indications
- Head not engaged.
- Brow presentation.
- Dead foetus perform an embryotomy (Chapter 9, Section 9.7).
- Cervix not fully dilated.
- Severe cephalo-pelvic disproportion, with head above the symphysis by more than 2/5 (Figure 5.17).
Figure 5.17 - Position of the foetal head
5.7.4 Equipment
- Scalpel, suturing equipment, delivery set with episiotomy scissors
- Vacuum extractor
- Foley catheter
- Sterile drape, compresses and gloves
- 10% povidone iodine
- 1% lidocaine
5.7.5 Technique
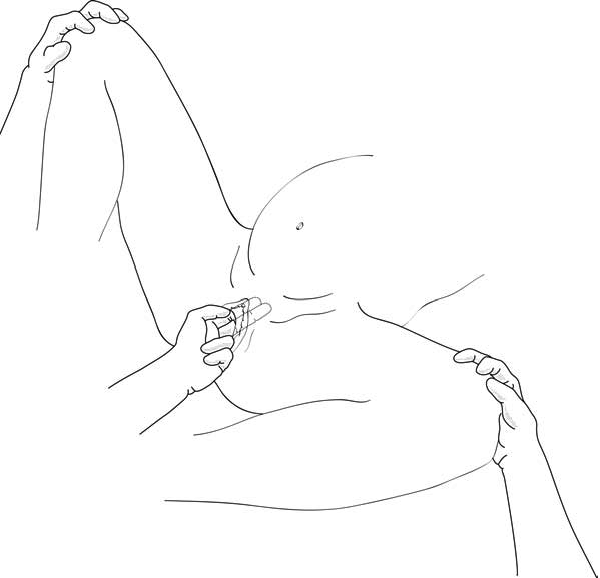
- Patient in lithotomy position, abduction supported by two assistants who maintain an angle of less than 90° between the patient's thighs (Figure 5.18).
Figure 5.18 - Supported lithotomy position
- Shave the incision site; swab the pubic and perineal region with 10% povidone iodine.
- Place a sterile fenestrated drape over the symphysis.
- Insert the Foley catheter, which allows location of the urethra throughout the procedure.
- Local anaesthesia: 10 ml of 1% lidocaine, infiltrating the skin and subcutaneous tissues superior, anterior, and inferior to the symphysis, along the midline, down to the cartilage. Infiltrate the episiotomy region as well.
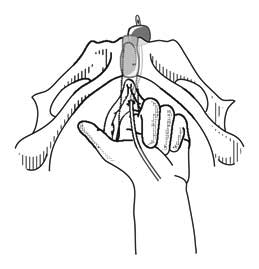
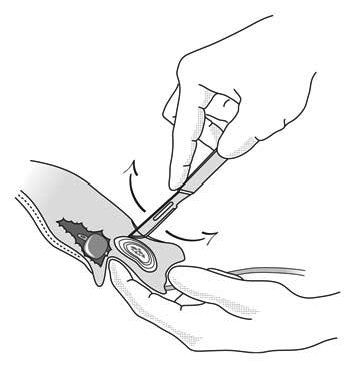
- With the index and middle fingers of the hand inserted into the vagina, push the urethra to the side (Figures 5.19 and 5.20). Place the index finger in the groove formed by the cartilage between the two pubic bones, in such a way that it can feel the scalpel's movements. The catheterized urethra must be pushed out of scalpel's reach.
Figure 5.19 - Finger pushing the urethra out of the way
Figure 5.20 - Finger pushing the head and urethra out of the way
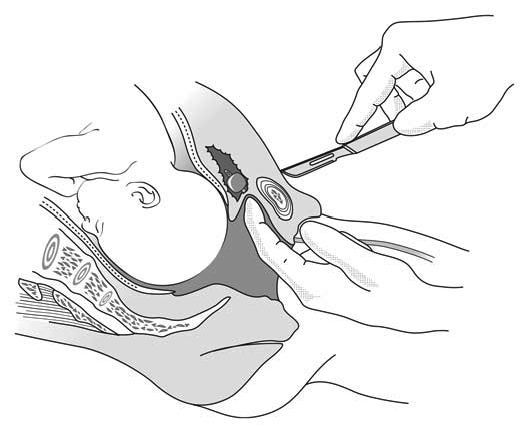
- Incision:
- Locate the upper edge of the symphysis.
- Introduce the scalpel 1 cm below this point, perpendicular to the skin, exactly on the midline.
- Cut down until the cartilage: it should feel elastic; if it feels bony, gently withdraw the blade and recheck the location.
- First tilt the blade toward the top, use a small back-and-forth motion (Figure 5.21), always along the midline, and in that way section 2/3 of the cartilage to the upper edge of the symphysis, going slightly past it.
- Then, turn the blade around toward the bottom, and repeat the sectioning manoeuvre down to the lower edge. The procedure is complete when the pubic bones move apart. The assistants continue to hold apart the thighs making sure they do not move further apart: the widening of the symphysis pubis must not exceed 2 to 2.5 cm (the width of a thumb).
Figure 5.21 - Scalpel moves back and forth
- Do not cut the vagina.
- Perform an episiotomy; use a vacuum extractor to deliver the neonate.
- One or two stitches suffice to close the wound after delivery.
5.7.6 Post-operative care
- Have the mother rest on her side (avoid forced abduction of the thighs) for 7 to 10 days. Mobilization with aid is possible as of Day 3 if the woman can tolerate the discomfort. No heavy work for 3 months.
- Remove the Foley catheter after 3 days, except if haematuria present during catheterization or in case of obstructed labour (Chapter 7, Section 7.2.5).
- Routine treatment for pain as for caesarean section (Chapter 6, Section 6.4.5).
5.7.7 Complications
- Bleeding at the site of the wound: compression bandage.
- Local infection: daily dressings and antibiotherapy (amoxicillin PO: 1 g 3 times daily for 5 days).
- Stress incontinence: uncommon and temporary.
- Gait problems: prevented through bed rest.
- Injury to the urethra or bladder: leave the catheter in place for 10 to 14 days and consult a specialist.
- Osteomyelitis: extremely rare if rigorous sterile technique has been used.
Notas
- (a)Caesarean section is not feasible because surgical conditions are inadequate or surgical intervention would take too long or there is a high risk of trauma to mother and foetus or the woman refuses caesarean section.