See Toolbox
Case definitions, triage and treatment
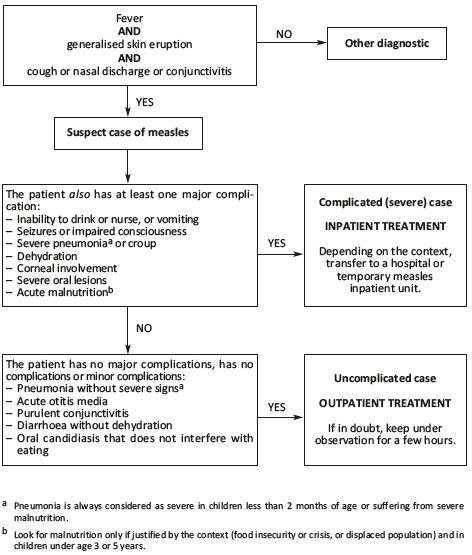
Uncomplicated cases (outpatient treatment)
Standard treatment
- Paracetamol PO: 20 mg/kg 3 times daily
Age < 2 months 2-11 months 1-4
years
5-10 years 11-15 years Adult Weight < 5 kg 5-9 kg 10-17 kg 18-32 kg 33-47 kg Oral sol. 120 mg/5 ml 3 ml
x 3
4 to 10 ml
x 3
– – – – 100 mg tab 3/4 tab
x 3
1 to 2 tab
x 3
2 to 3 tab
x 3
– – – 500 mg tab – – ½ tab
x 3
½ to 1 tab
x 3
1½ to 2 tab
x 3
2 tab
x 3
- Amoxicillin PO: 25 to 50 mg/kg 2 times daily for 5 days in children under 5 years
Age < 2 months 2-11 months 1-4 years Weight < 5 kg 5-9 kg 10-17 kg Oral susp. 125 mg/5 ml ½ tsp x 2 2 to 3 tsp x 2 – 250 mg tab 1 tab x 2 1 to 2 tab x 2 2 to 3 tab x 2 500 mg tab – – 1 to 2 tab x 2
- Retinol* (vitamin A) PO: one dose on Day1
Age < 6 months 6-11 months 1 year and over Weight < 7.5 kg 7.5-9 kg 10 kg and over Dose 50 000 IU 100 000 IU 200 000 IU 200 000 IU capsule
(8 drops)2 drops 4 drops 1 capsule
* except in pregnant women
- Wipe eyes with cotton and clean water.
- Keep nasal passages clear (using a tissue or by nasal lavage with 0.9% sodium chloride if appropriate).
- Depending on the context, for children < 3 or 5 years, food supplement: 500 kcal daily, ready-to use food, 2 weeks.
Treatment of complications
- Pneumonia without severe signs or acute otitis media: amoxicillin PO 5 days
- Purulent conjunctivitis: clean the eyes with clean water + tetracycline eye ointment 1% (2 times daily, 7 days)
- Bitot’s spots: retinol PO one dose on Day1, Day2, Day8
- Oral candidiasis: nystatin 100 000 IU/ml oral suspension (1 ml 4 times daily, 7 days) aCitation a.If not available, 0.25% gentian violet, applied 2 times/day for 5 days maximum.
- Diarrhoea without dehydration: WHO plan A
|
Complicated cases (inpatient treatment)
Standard treatment
- Paracetamol PO: 20 mg/kg 3 times daily
Age < 2 months 2-11 months 1-4
years
5-10
years
11-15
years
Adult Weight < 5 kg 5-9 kg 10-17 kg 18-32 kg 33-47 kg Oral sol. 120 mg/5 ml 3 ml
x 3
4 to 10 ml
x 3
– – – – 100 mg tab 3/4 tab
x 3
1 to 2 tab
x 3
2 to 3 tab
x 3
– – – 500 mg tab – – ½ tab
x 3
½ to 1 tab
x 3
1½ to 2 tab
x 3
2 tab
x 3
- Only in case of high fever in a child who is vomiting repeatedly or whose consciousness is impaired, paracetamol IV, 500 mg vial (10 mg/ml, 50 ml
Weight < 10 kg 10-50 kg > 50 kg Dose to be administered
every 6 hours (in mg)7.5 mg/kg 15 mg/kg 1 g Dose to be administered
every 6 hours (in ml)0.75 ml/kg 1.5 ml/kg 100 ml Dose maximum 30 mg/kg/day 60 mg/kg/day 4 g/day
Administer paracetamol IV in 4 doses at 6-hour intervals. Each dose is administered over 15 minutes. Change to oral route as soon as possible.
- Amoxicillin PO: 25 to 50 mg/kg 2 times daily for 5 days in children under 5 years
Age < 2
months
2-11
months
1-4
years
5-10
years
11-15
years
Adult Weight < 5 kg 5-9 kg 10-17 kg 18-32 kg 33-47 kg Oral susp. 125 mg/5 ml
1½ tsp
x 2
2 to 3 tsp
x 2
– – – – 250 mg tab 1 tab
x 2
1 to 2 tab
x 2
2 to 3 tab
x 2
– – – 500 mg tab – – 1 to 2 tab
x 2
2 to 3 tab
x 2
3 to 4 tab
x 2
4 tab
x 2
- Retinol (vitamin A) PO: one dose on Day1 and Day2
Age < 6 months 6-11 months 1 year and over Weight < 7.5 kg 7.5-9 kg 10 kg and over Dose 50 000 IU 100 000 IU 200 000 IU 200 000 IU capsule (8 drops) 2 drops 4 drops 1 capsule
Administer retinol PO in 2 doses (Day1, Day2) to all patients except:
- pregnant women (contra-indicated);
- in the event of corneal lesions or Bitot’s spots (in this case, give 3 doses, on Day1, Day2, Day8).
- Wipe eyes with clean water 2 times daily.
- Keep nasal passages clear (using a tissue or by nasal lavage with 0.9% sodium chloride if appropriate).
- Give caloric food, smaller, more frequent meals or breastfeed more frequently.
- Make the child drink regularly.
- Depending on the context, for children < 3 or 5 years, food supplement: 500 kcal daily, ready-to use food, 2 weeks.
Respiratory and ENT complications
Severe pneumonia
- Oxygen if cyanosis or SpO2 < 90%
- Ceftriaxone slow IV or IM (1 g to be dissolved in 5 ml): 100 mg/kg once daily
Age 1-11
months
1-4
years
5-10
years
11-15
years
Adult Weight 4-9 kg 10-17 kg 18-32 kg 33-47 kg Dose 400 to 900 mg 1 to 1.5 g 2 to 3 g 3 to 4 g 4 g Volume to be injected
(1 g vial /5 ml of diluent)2 to 5 ml 1 to 1½ vial 2 to 3 vials 3 to 4 vials 4 vials
IV injection:
When ceftriaxone is administered by IV route, the powder (1 g) must be dissolved in 5 ml of water for injection.
IM injection:
Vials of ceftriaxone for IM injection are provided with a specific diluent containing lidocain. Once reconstituted with this diluent, ceftriaxone can be administered by IM route only, NEVER BY IV ROUTE. Doses (in ml or vials) in the table above are based on a ceftriaxoneconcentration of 1 g diluted in 5 ml of diluent with lidocain. Always verify the dosage and the volume of diluent as they can vary according to the manufacturers (500 mg/2 ml, 500 mg/5 ml, 1 g/5 ml, 1 g/10 ml, etc.). All of the diluent must be used for reconstitution. If the volume to be injected is large, administer half the dose into each buttock.
PLUS
- Cloxacillin IV infusion over 60 minutes (500 mg to be dissolved in 5 ml water for injection): 25 to 50 mg/kg every 6 hours
Age < 2
months
2-11
months
1-4
years
5-10
years
11-15
years
Adult Weight < 5 kg 5-9 kg 10-17 kg 18-32 kg 33-47 kg Dose 200 mg
x 4
250 to 400 mg
x 4
500 to 750 mg
x 4
1 g
x 4
1.5 g
x 4
2 g
x 4
Volume to be injected
(500 mg vial /5 ml)2 ml
x 4
2.5 to 4 ml
x 4
1 to 1½ vial
x 4
2 vials
x 4
3 vials
x 4
4 vials
x 4
Parenteral treatment for at least 3 days then, once the child no longer has fever or clinical signs of severe infection, change to amoxicillin/clavulanic acid PO: 40 mg/kg 2 times daily to complete 7 to 10 days of treatment
| Age |
< 2 months |
2-11 months |
1-4 years |
5-10 years |
11-15 years |
Adult |
|---|---|---|---|---|---|---|
| Weight | < 5 kg | 5-9 kg | 10-17 kg | 18-32 kg | 33-47 kg | |
|
Oral susp. 100 + 12.5 mg/5 ml |
8 ml x 2 |
12 ml x 2 |
– |
– | – | – |
| 500/62,5 mg tab | – | – |
1 tab x 2 |
2 tab x 2 |
3 tab x 2 |
3 tab x 2 |
Pneumonia (without signs of severity)
- Amoxicillin PO: 25 to 50 mg/kg 2 times daily for 5 days
Age < 2
months
2-11
months
1-4
years
5-10
years
11-15
years
Adult Weight < 5 kg 5-9 kg 10-17 kg 18-32 kg 33-47 kg Oral susp. 125 mg/5 ml
1½ tsp
x 2
2 to 3 tsp
x 2
– – – – 250 mg tab 1 tab
x 2
1 to 2 tab
x 2
2 to 3 tab
x 2
– – – 500 mg tab – – 1 to 2 tab
x 2
2 to 3 tab
x 2
3 to 4 tab
x 2
4 tab
x 2
As a second line (treatment failure after 48 hours), amoxicillin/clavulanic acid PO: 40 mg/kg 2 times daily for 7 days (see Severe pneumonia).
Acute otitis media
- Amoxicillin PO: 25 to 50 mg/kg 2 times daily for 5 days (see above)
- If there is discharge from the ear, keep the ear clean by wiping the external auditory canal with dry cotton wool.
Severe laryngotracheobronchitis (croup)
- Dexamethasone (1 ml ampoule, 4 mg/ml) IM: 0.6 mg/kg single dose
Age < 2 months 2-11 months 1-4 years 3-4 years Weight < 5 kg 5-9 kg 10-13 kg 14-17 kg Dose 2 mg 4 mg 8 mg 10 mg Volume to be injected 0.5 ml 1 ml 2 ml 2.5 ml
- Nebulized epinephrine (1 mg ampoule, 1 mg/ml): 0.5 ml/kg per dose
Age 1
month
2
months
3
months
4-6 months 7-9 months 10-11 months 1-4 years* Weight 4.5 kg 5 kg 6 kg 7 kg 8 kg 9 kg 10-17 kg Epinephrine
(1 mg/ml ampoule)2 ml 2.5 ml 3 ml 3.5 ml 4 ml 4.5 ml 5 ml 0.9% NaCl to be added 2 ml 2 ml 1 ml 1 ml – – –
* In children > 4 years or > 17 kg, the dose should not exceed 5 ml.
- Oxygen if cyanosis or SpO2 < 90%
Ocular complications
Corneal lesions (opacification, ulcer)
- Retinol (vitamin A) PO: one dose on Day1, Day2, Day8
Age < 6 months 6-11 months 1 year and over Weight < 7.5 kg 7.5-9 kg 10 kg and over Dose 50 000 IU 100 000 IU 200 000 IU 200 000 IU capsule (8 drops) 2 drops 4 drops 1 capsule
- Tramadol PO if ocular pain:
- Child over 12 years and adult: 50 to 100 mg every 6 hours (max. 400 mg daily)
Age > 12 years Adult Dose 50 mg x 4 100 mg x 4 Gél 50 mg 1 cap x 4 2 cap x 4
- Child over 12 years and adult: 50 to 100 mg every 6 hours (max. 400 mg daily)
- Keep the eye clean: clean with 0.9% sterile sodium chloride and apply tetracycline eye ointment 1%, 2 times daily, to prevent or treat bacterial superinfection.
- Protective dressing as long there is photophobia.
Bitot’s spots
- Retinol (vitamin A) PO: one dose on Day1, Day2 and Day8, as above
Purulent conjunctivitis
- Clean the eyes with clean water 2 times daily.
- Tetracycline eye ointment 1%: one application 2 times daily for 7 days
Gastrointestinal complications
Oral candidiasis
- Nystatin PO: 1 ml of oral suspension (100 000 IU) 4 times daily for 7 days aCitation a.If not available, 0.25% gentian violet, applied 2 times/day for 5 days maximum. . If there is no improvement after 3 days, increase the dose to 200 000 IU 4 times daily.
Diarrhoea without dehydration
WHO treatment plan A
Diarrhoea with dehydration
- Rehydration:
Moderate (some) dehydration: WHO treatment plan B
Severe dehydration: WHO treatment plan C
+
- Zinc sultate (20 mg dispersible tablet):
- Child under 6 months: 10 mg once daily for 10 days (= ½ tab daily)
- Child from 6 months to 5 years: 20 mg daily for 10 days (= 1 tab daily)
In infants: place ½ or 1 tablet in a teaspoon and add a bit of water to dissolve it.
In children over 2 years: tablets may be chewed or dissolved.
Ask the parents not to remove the tablets from the blister-pack. Once a tablet is removed from the blister-pack, it must be administered immediately.
Other complications
Acute malnutrition
Follow the protocol for managing malnutrition (RTUF).
Seizures
Generalised seizure lasting > 3 minutes:
- diazepam: 10 mg ampoule (5 mg/ml, 2 ml)
Child: 0.5 mg/kg rectally, without exceeding a total dose of 10 mg
- For intrarectal administration, use a 1 ml-syringe graduated in 0.01 ml (with no needle). Introduce the tip of the syringe into the rectum (1.5 to 4 cm depending on age).
Age < 4 months 4-11 months 1-2 years Weight < 7 kg 7-9 kg 10-13 kg Dose in mg
2.5 mg 4 mg 6 mg Volume to be administered 0.5 ml 0.8 ml 1.2 ml
If seizures persist after 5 minutes after the first dose, repeat the same dose once.
If the patient is to be transferred to a hospital
- Administer the first dose of amoxicillin PO and paracetamol PO.
- Severe dehydration: place a IV line and transfer the patient when stable.
- Moderate (some) dehydration: the patient should be able to drink ORS while being transferred.
- Corneal lesion: protect the eye with a dry dressing.
- Send the patient with a transfer form indicating the reason for the referral and treatments administered.
- (a)If not available, 0.25% gentian violet, applied 2 times/day for 5 days maximum.